Conference Notes 4/16/13
Kettaneh/Felder Oral Boards
Case 1. Syncope due to Brugada syndrome. Pt also fractured humerus due to fall. Critical actions: Identify brugada and consult cardiology. Splint and manage fx. Brugada syndrome arrhythmias usually occur at rest.
Three types of Brugada waveform. 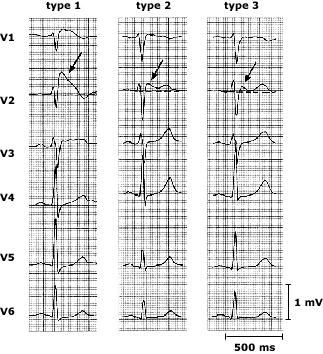 Three distinct types of ST segment elevation have been described. In type 1, the ST segment gradually descends to an inverted T wave. In type 2, the T wave is positive or biphasic, and the terminal portion of the ST segment is elevated ≥1 mm. In type 3, the T wave is positive, and the terminal portion of the ST segment is elevated <1 mm. Arrows denote the J-waves.
Three distinct types of ST segment elevation have been described. In type 1, the ST segment gradually descends to an inverted T wave. In type 2, the T wave is positive or biphasic, and the terminal portion of the ST segment is elevated ≥1 mm. In type 3, the T wave is positive, and the terminal portion of the ST segment is elevated <1 mm. Arrows denote the J-waves.
Case 2. Seizing patient due to hyponatremia from post-partum pituitary necrosis. Pt had intra-partum hemorrhage with hypotension and transfusion. This resulted in pituitary infarct/necrosis. Pt has been having difficulty lactating and has been weak. Critical actions: Hypertonic saline, antibiotics for uti, hydrocortisone. Consult appropriately. Sheehan syndrome consists of pituitary necrosis due to ischemia in the peripartum period.
Case 3. Seizing NH patient due to hypoglycemia. Pt accidentally received a dose of insulin intended for another patient. Critical actions: Identify hypoglycemia, IV glucose, feed, check serial blood sugars.
Elise comment: If there is a specific fx that causes a known neuro-vascular injury then specifically check for this injury. Example: midshaft humerus fx is associated with wrist drop. Specifically tell the examiner you want to examine for wrist extensor strength.
Harwood comment: You can get an insulin level on a patient to see if they received too much insulin. There can be varying severity of Sheehan’s syndrome. Mild cases can be difficult to diagnose. There is a website brugada.org that can give you some guidance on how to manage these patients. Incidental brugada cases identified in the ED should be referred to an EP specialist to see if an arrythmia can be induced. IF so, they will need an AICD.
Girzadas comment: Be alert for hyponatremia and mild hyperkalemia in a weak or hypotensive patient. This is usually adrenal insufficiency. Get a serum cortisol level and give hydrocortisone in stress doses.
Chandra M&M
Pt with fournier’s gangrene. Rapidly progressing necrotizing fasciitis of perineal/perianal/genital region. Usually in men around age 50-60. Diabetes and obesity increases the risk. Indwelling catheters, etohism, immunosuppression also increase risk. 
Can be caused by local infections like abscess, fissure, diverticulitis, etc. 10% of cases are idiopathic.
Look for scrotal pain, swelling, fever. Patient’s may have severe genital pain. Check for subcutaneous crepitation.
94% of cases involve the srotum, 47% involve the penis, and 35% of cases involve the perineum.
Fournier’s severity index: Basically SIRS plus lab abnormalities correlates with increased mortality. Elise comment: This index looks like unvalidated BS.
U/S can show subQ air but is less sensitive than CT. CT is most sensitive for subQ emphysema and can show source of infection and extent of spread. Harwood comment: Get fine cuts through scrotum and perineum. Less concerned about the rest of abdomen.
Treat with surgical debridement. Give triple antibiotics. Hyperbaric o2 is controversial and is used after surgical debridement. 24 hour delay in surgery increases mortality by 11%. Mean hospital stay is 30 days.
Pitfalls: Have high suspicion for this rapidly progressive diagnosis. Sign outs increase risk. Push back against consultant bias that downplays disease process.
Girzadas comment: During sign out make sure there is some back and forth discussion between teams about these high risk patients. Harwood comment: Be careful to not just say “nothing to do”. Rather you need to say, you have to re-examine the patient’s scrotum. Question whether the antibiotics have been written for repeated doses if they are boarding for a prolonged time in the ED. Elise comment: Identify your sickest patient and highlight the need for further attention. DenOuden comment: Bedside sign out may be helpful in these high risk cases. Harwood comment: These guys need serial exams because it can be “awe inspiring to see how fast this can progress”. Christine comment: Ct is very important in these diagnoses. Harwood comment: MRI is the most sensitive test for necrotizing fasciitis.
Paarul comment: Prior to sign out review your orders for critically ill patients.
Harwood comment: This case was due to a system error. Our EMR takes so many clicks to place orders, it increases your risk of error. Elise comment: It is ok to push back professionally against consultants if you feel strongly the patient needs a certain intervention. Kelly Williamson comment: We train for worst case scenarios and are constantly alert for them. Consultants frequently down play a disease process. You have to be aware of this difference in perspective. Willison comment: Inturruptions also increase our risk for error. Joan Coghlan comment: signouts are made more difficult also by the arduousness of the EMR system.
Kettaneh Tranexamic Acid in the ED
TXA is a synthetic analog of lysine. It competitively inhibits the activation of plasminogen to plasmin.
Common minor Adverse effects: abdominal pain, arthralgia, headache, fatigue.
CRASH-2 study: 40 countries with 20,000 trauma patients. Showed lower all cause mortality.
MATTERs study: showed lower mortality in TXA group.
ICH study: showed trends to less ICH growth and lower mortality.
Re-analysis of CRASH-2 showed the earlier you give TXA the better the effect. Want to give in less than 3 hours.
Give to Trauma patients with hypotension or tachycardia or expected need for transfusion. Until further research, don’t give to isolated head trauma patients.
Dose is 1g IVPB over 10min followed by 1g IVPB over 8 hours.
PharmD comment: This is a benign drug. It is not a pro-coagulant. It only stabilizes the clotting system. Elise comment: This drug provides a modest but real benefit in bleeding trauma patients There was consensus that we should be using this in multisystem trauma patients with bleeding, hypotension, tachycardia, or need for transfusion.
Kettaneh Case F/U
63yo male with presyncope. Sob and diaphoretic after lifting a pallet. His wife made him go to the ER.
Which is a clear marker for bad pathology. Harwood comment: Another marker for bad pathology is when long time smokers spontaneously stop smoking. When a patient tells him they recently stopped smoking on their own, he gets worried. Vitals showed tachycardia. EKG showed sinus tachycardia with subtle inferior st changes.
Pt became hypotensive in the ED. Bedside echo shows moderate pericardial effusion with good contractility. No chest or back pain. Dimer is elevated. Second EKG looks better.
To diagnose cardiac tamponade , tachycardia is almost always present. JVD is commonly present. Electrical alternans is an EKG finding specific but insensitive for tamponade.
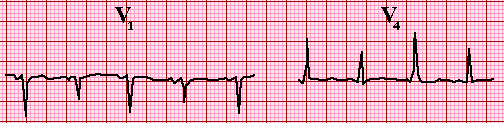
Electrical alternans.
U/S will show diastolic collapse of RV when tamponade is present.
CTA of this patient showed an aortic dissection and no PE.
Type A in Standford classification involves ascending aorta. Type B means only descending aorta.
This patient had a painless Type A dissection. 6% of aortic dissection patients have no pain. These patients with painless dissections are more likely to have syncope, stroke symptoms or CHF symptoms.
Patient went to OR and had repair of ascending dissection and aortic valve replacement.
Nick felt the dimer may have saved the patient’s life. Kari Tekwani recently diagnosed a relatively painless dissection on another patient and she also felt the dimer helped pick up the dissection.
Harwood comment: If you aren’t sure if the diagnosis is pe or dissection go with the CT PE rather than CTA study. You probably won’t miss a significant dissection on a CT PE study. If you do a CTA aorta study, you will miss many pe’s.
Watts Vent Management Software Demonstration
Cash 5 Slide F/U
91 yo female with altered mental status. Dexi was 56 in the field. Pt was hypothermic and hypertensive. Cachectic and dehydrated.
Labs c/w urosepsis. Pt became more hypothermic and became hypotensive. Diagnosis was urosepsis.
Started on Cetriaxone and Levophed. IM brought up possibility of myxedema coma. EM clinicians considered diagnosis but felt the expected doughy appearance of a myxedema patient was not present. Pt’s TSH was later found to be 250. Diagnosis was made of myxedema coma.
Hallmarks of myxedema coma are: mental status change, hypothermia, bradycardia, hyponatremia, hypoglycemia, hypotension, and precipitating illness.
Treat with levothyroxine, hydrocortisone to cover possible adrenal insufficiency. Manage hypoglycemia, manage hypotension, provide passive re-warming, and monitor for arrhythmias.
Beckemeyer 5 slide F/U
79 yo female with sudden onset headache and neck pain with emesis. Pt has afib and is on Coumadin.
ED clinicians ordered CTA of head and neck. Pt was found to have a right MCA aneurysm with diffuse SAH. Pt was given FEIBA to reverse Coumadin and then went to neurointerventional lab and had aneurysm coiled. Pt was dc’d home with no focal deficits. Badabing Badaboom!