Conference Notes 10-15-2014
Carlson Study Guide Toxicology
Best treatment for TCA induced cardiac dysrhythmias is sodium bicarb. TCA’s are “dirty drugs”, meaning they have multiple mechanisms of action.
*TCA toxicity
You can differentiate sympathomimetic toxidrome vs anticholinergic toxidromes by checking for diaphoresis in the arm pits and hypertension. Both suggest sympathomimetic toxidrome. Urinary retention suggests anticholinergic toxidrome.

*Toxidromes
Lithium is renally excreted. Anything affecting the kidneys such as a diuretic or renal failure will increase lithium levels. As a memorable illustrationg, Andrea described a case of a patient who by drinking his own urine maintained a high lithium level while an inpatient.
Multidose activated charcoal is indicated for phenobarbital overdose.
Lorazepam and Midazolam have predictable IM absorption. Diazepam does not. Use lorazepam or midazolam if you need to treat a seizure and don’t have an IV.
Simplified Osmolal Gap Calculation= 2NA + BUN/3 + Glucose/20 + ETOH/5
Diphenhydramine toxicity looks a lot like and is treated similarly to TCA overdose.
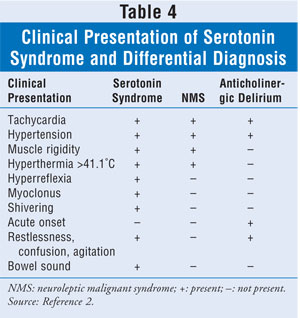
Treatment for neuroleptic malignant syndrome includes bromocriptine, dantrolene, and benzodiazepines. Cyproheptadine is indicated for serotonin syndrome.
*NMS vs Serotonin Syndrome
There are no false positives for urine testing for cocaine. No other drugs will cause a false positive result.
For adequate urinary alkalinization, correction of hypokalemia is essential. With hypokalemia the kidney will not alkalinize the urine even when you give bicarb.
Lithium does not bind to activated charcoal.
Flumazenil can reverse sedation caused by ambien.
Methanol is metabolized to formic acid and ethylene glycol is metabolized to glycolic acid.
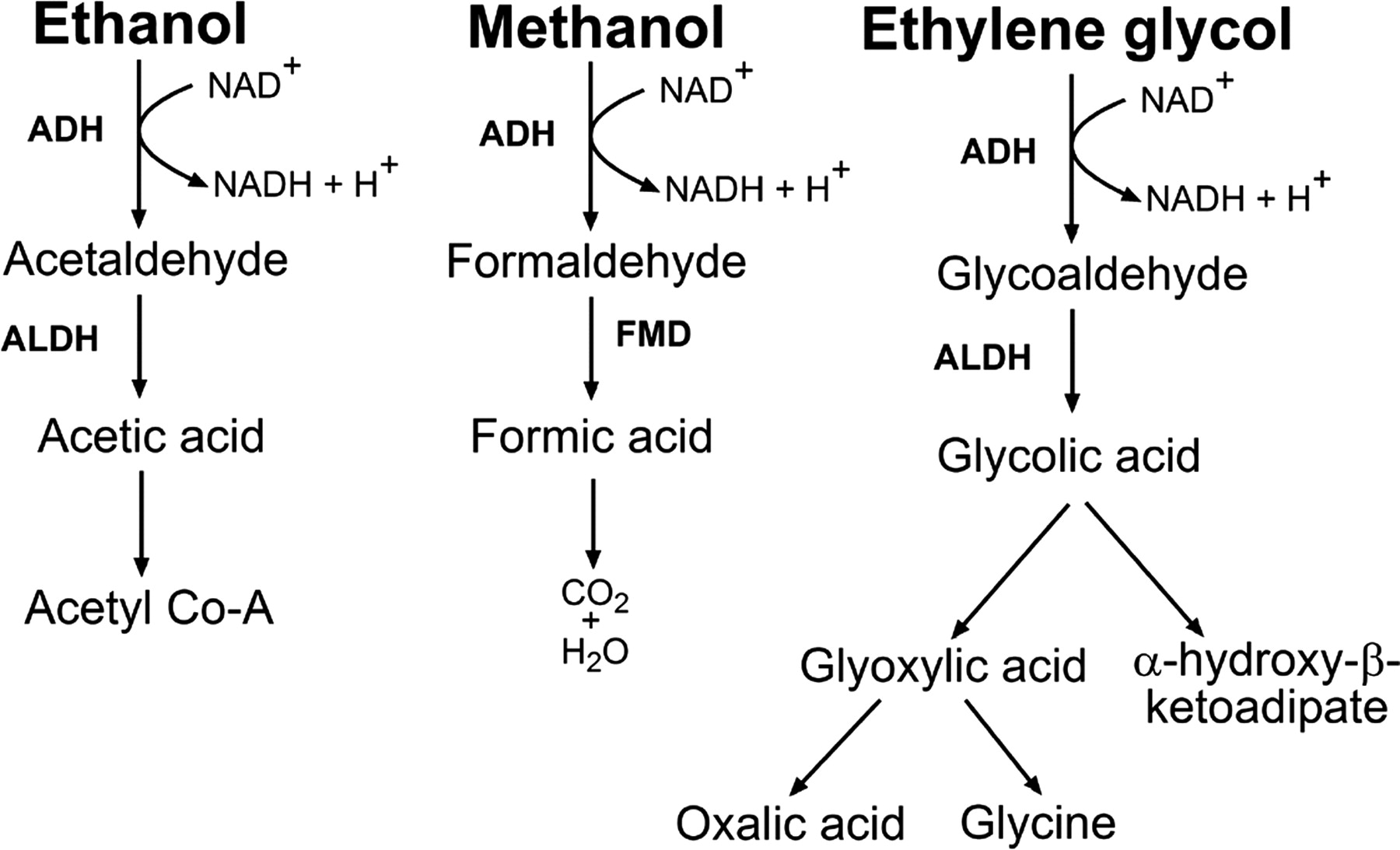
* Toxic Alcohol Metabolites
Naloxone’s duration of action is about an hour. Andrea suggests watching a heroin overdose patient for about 4 hours. She will let a heroin user sign out AMA after about an hour or so. You have to be very clear with a heroin user who is signing out that there is still some narcan in their body and using heroin in the next few hours is very dangerous. They potentially may use a higher dose of heroin in order to overcome the effects of the residual narcan and when the narcan clears, they could have a respiratory arrest.
Navarette DKA
Type 2 DM has a strong familial link. Halle Berry was diagnosed with type 2 dm. So it is not just overweight middle age adults that get type 2 DM.
2 large bore IV’s should be placed in the DKA patient. Ask the nurse to place an 18g catheter or larger.
DKA is a problem of too little insulin. There is also too much counter-regulatory hormones. Lowering the serum glucose level is not enough, these patients need adequate insulin dosing until their acidosis clears. IV fluids dilute the counter-regulatory hormones.
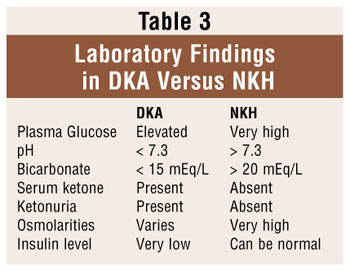
DKA and Hyperosmolar Coma have some overlap. The difference is a matter of degree not a fundamentally different pathophysiology. Hyperosmolar coma is less common, has a higher mortality, and has a greater degree of dehydration. Hyperosmolar coma patients have some minimal residual insulin production so they don’t get as ketotic or develop a significant gap.
*DKA vs Hyperosmolar Coma
Give IV fluids: In adults, 1 liter initial bolus is reasonable. Then give another liter over the next 2 hours. Cerebral edema is a risk but is more common in kids with severe acidemia than adults. You have to be a little bit cautious with fluids in adults and more cautious with fluids inin kids. It is best to follow a DKA protocol to not over-hydrate.
Diagnosis of cerebral edema includes 3 major criteria: altered mental status, bradycardia, incontinence. 3 minor criteria: vomiting, headache, and lethargy
Harwood and Girzadas comments: The higher risk patients for cerebral edema are kids with more severe acidosis. You have to be really careful with fluids in these patients. Use of a DKA protocol is important. Bicarb use is another risk factor and as bicarb has been taken out of DKA protocols the incidence of cerebral edema has gone down.
Hypokalemia is a big risk when managing DKA. You have to be very attentive to potassium changes.
Girzadas comment: There have been cases of patients dying from hypokalemia during treatment of DKA. You need to follow the DKA protocol carefully and need to be attentive to any downtrending of potassium levels.
DKA is a problem of lack of insulin. Start insulin drip at 0.1 u/kg/hr. No bolus of insulin is indicated. Do not stop insulin until HCO3 is >18, AG<12, or pH>7.3. Don’t stop the insulin drip for hypoglycemia if these other endpoints have not been reached. Treat hypoglycemia and slow but don’t stop insulin drip.
For anion gap calculations, use the measure sodium. Don’t use a sodium level corrected for hyperglycemia.
VBG is good enough to guide management. You don’t need an ABG.
Rapid-acting insulins are novolog and humulog. Patients use this for glucose control at meal times. Long acting insulin (lantus) should be on board as well around the clock for a basal level of insulin control.
Insulin pumps are tailored to each specific patient. It allows very tight management of blood sugar. Interestingly, patients on pumps tend to go into DKA more frequently than non-pump patients. This is because if the pump fails for some reason, the patient has no insulin on board at all. Patients using shots have lantus insulin on board that will keep sugar down somewhat. Pump patients don’t have any lantus or other long-acting insulin on board.
Glucagon does not work for intoxicated hypoglycemic patients. The liver is metabolizing alcohol and can’t convert glucagon to glucose. You have to give IV glucose to correct hypoglycemia in hypoglycemic patients with an elevated blood alcohol level.
Gore ACEP CPC Case Presentation
Have to keep the case a secret until ACEP. Please go the CPC National Finals at ACEP Monday morning 10-27-2014 to see Kasia Gore win it!
Cirone ACEP Research Presentation
Mike Cirone is presenting Tuesday morning 10-28-2014 at ACEP in the Infectious Disease section. Please attend his presentation if you are attending ACEP.
Retrospective study evaluating urine culture results from ED and Urgent Care settings. Ecoli was #1 identified pathogen and klebsiella was #2. In ED patients, Ecoli was most susceptible to macrobid and Keflex. Cipro and Bactrim functioned below the 80% susceptibility level. In the urgent care settings, the antibiotic resistance levels were less than in the ED and all 4 antibiotics (macrobid, Keflex, cipro, and Bactrim) worked above the 80% effectiveness rate. The usual antibiogram you see from your institution combine sensitivities from all body fluid sources (blood, sputum, urine, pus). If you can break them out you get different sensititivities for different body fluid sources.
Purnell ACEP Research Presentation
Lindsay Purnell is presenting at ACEP as well. Please refer to the ACEP Meeting info for her time of presentation.
Prospective study evaluating two patient assignment models in the ED. We compared a geographic model (each physician covers a specific group of beds in the ED) vs a rotational assignment model (patients are assigned to physicians according to a rotation system). Time to first provider and time to disposition were actually better in the geographic model. Length of stay, time to nurse, and time to bed showed no significant difference between the groups.
Htet ACEP Research Presentation
Natalie Htet is presenting on Tuesday 10-27-14 at ACEP between 1:30p and 3p.
A Prospective multi-center observational study of ultrasound for management of pediatric soft tissue infections was described. The data collection is currently ongoing. It is hoped that ultrasound at the point of care will improve the sensitivity and specificity of diagnosing soft tissue infections (abscesses vs. cellulitis).
Jeziorkowski Anal/Rectal Emergencies
Hidradenitis: A keratin plug blocks a hair follicle. Bacteria multiply in the apocrine sweat gland. The gland ruptures and spreads bacteria. Cause is unknown. Treat with topical clindamycin or oral doxycycline. Incision and drainage can relieve pain and swelling but does not alter the course of the disease.
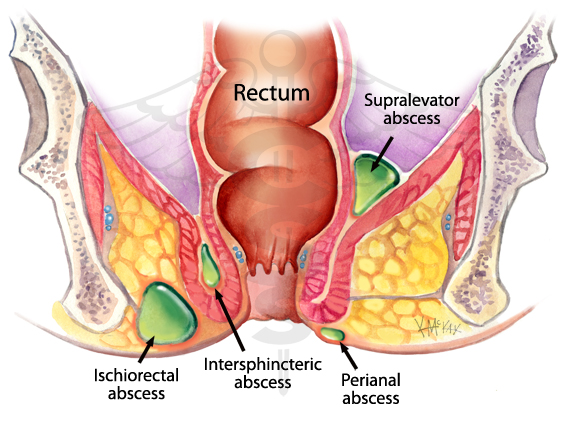
Perirectal abscess: There is a spectrum of severity. Perianal abscess is the least severe/most common and can be drained in the ED. Next is the ischiorectal abscess located laterally to the anus and medial to buttock. These require OR drainage. Interphincteric abscess has no external signs and require OR drainage. Supralevator abscesses will have severe perianal pain, fever , and possibly urinary retention. These also need to be drained in the OR. Finally is the horseshoe abscess that is the least common and requires OR drainage.
Give antibiotics for all types of these abscesses if the patient has any immunocompromise.
*Perirectal abscess types
Rectal prolapse: Sedate and reduce. If you can’t reduce, consult surgery.
Anal fissure: Treat with sitz baths, increase fiber in diet, wash frequently. Most anal fissures are in posterior midline. If you see it away from the posterior midline in a child think inflammatory bowel disease. If you see a fissure in an adult out side the posterior midline, think crohn’s, TB, or syphillis.
Hemorrhoids: If the hemorrhoid is thrombosed, it will be painful. If present more than 48 hours consider conservative management with sitz baths, bulk laxatives and pain relief. Pain most commonly will be improving after that time frame. If the thrombosed hemorrhoid is present less than 48 hours then excision of the clot is most likely indicated.
Harwood comment: If you have a thrombosed external hemorrhoid they won’t bleed much after making an elliptical incsion. I pull up the skin overlying the hemorrhoid and cut a piece of skin with scissors to create an elliptical incision. Girzadas comment: This is a great ED case. You can give patients a lot of pain relief and you get the satisfaction of removing a discrete clot. It is a procedure that is better than draining an abscess. You have to be careful that you are truly cutting into a thrombosed hemorrhoid. Look for a purple hue under the skin and you can feel a firm clot with your finger tips.
*Thrombosed Hemorrhoid
Rectal FB: Can be difficult to manage. Most faculty present recommended consulting surgery or GI for anything beyond a small object that is not that far in the rectum. There is a risk of perforation in these cases.
Kmetuk Pediatric Respiratory Emergencies
Epiglotitis: Treat with racemic epi, antibiotics (Ceftriazone), mobilize anesthesia and ENT to provide airway management in the OR. If you have to attempt intubation, use a tube one size smaller than recommended by broslow or other sizing tools. Girzadas comment: If you have an airway disaster it is thought that you can bag-valve-mask ventilate the patient with epiglottitis. This can buy you some time. If you can’t intubate, attempt needle cricothyrotomy.
Best modality to diagnose retropharyngeal abscess is CT with IV contrast. Treat with IV unasyn or clindamycin. Consult ENT for possible surgical management.
Croup: Treat with decadron po and consider racemic epi. Admit for persistent stridor, need for multiple doses of racemic epinephrine, respiratory distress, or hypoxia.
Bacterial tracheitis: Initially the clinical picture looks like croup but kids rapidly deteriorate and become toxic. Treat with ceftriazone, plus clindamycin or vancomycin. Most kids need intubation.
Bronchiolitis: Treatment options include: O2 if needed, suctioning, albuterol, racemic epinepherine, 3% hypertonic saline nebs, and consider bipap or intubation for severe cases.
Admission criteria include 02 sat less than 95%, premie who is less than 6 months, any child less than 12 weeks of age, apnea, tachypnea more than 60, unable to feed due to respiratory effort. Other factors that may increase the risk of admission are presentation with less than 5 days of symptoms and heart rate above 160.
John Paik referred reference: Administration of nebulized 3% saline in the emergency department did not result in a statistically significant decrease in the rate of admission for infants presenting with acute bronchiolitis, though there was a trend towards decreased admissions in both outpatient studies. However, in the studies examining inpatients, infants in the treatment arms had an average decrease in hospital stay of approximately 1 day, with no adverse reactions or harms recorded. Subjects receiving 3% saline were also noted to have improved clinical severity scores, especially on the first day of admission, when compared to the groups receiving 0.9% saline.
Pertussis can be treated with azithromycin, erythromycin, or Bactrim. Similar admit criteria to bronchiolitis.
Airway FB: 75% of airway FB’s are radiolucent. Inspiratory and expiratory films can be helpful to identify whether a FB is present. With a mainstem bronchus FB there will be air trapping on that side with expiration.
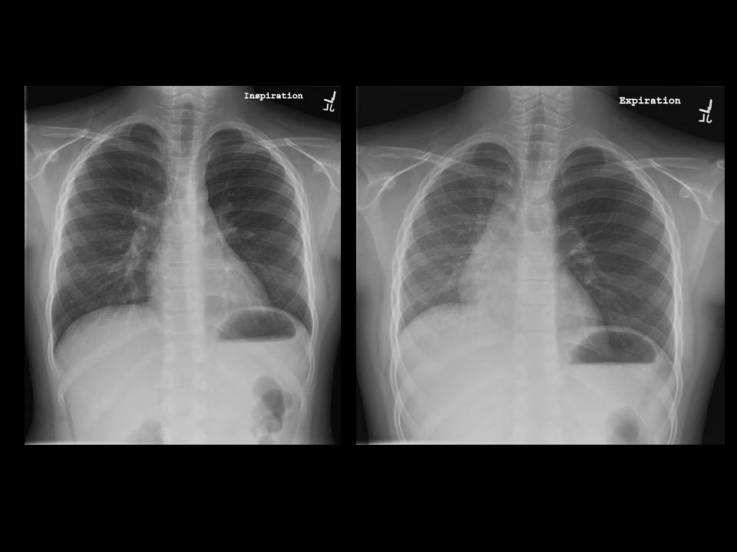
*Inspiratory/Expiratory CXR. Air trapping in the left hemithorax on expiratory film
Christine Kulstad comment: The pneumonia protocol for kids older than 90 days at ACMC is Ceftriazone and Azithromycin for inpatients and Augmentin or Azithromycin for outpatients. Girzadas comment: Up to Date says admit all kids with pneumonia under 6 months. After six months, if you decide to treat as an outpatient your options are amoxicillin, augmentin, cefdinir, or azithromycin.
For severe asthma consider terbutaline, aminophilin, ketamine, heliox, and bipap in addition to aggressive albuterol and steroids.
Criteria for PICU admission: severe asthma, continuous albuterol for 3 hours, continuous supplemental O2 >40% FIO2, and any child who is tiring out.
Girzadas PPE for Patients with suspected Ebola
#1 Message: Screen all patients presenting with fever, headache, or GI symptoms for recent travel to a high risk West African country(Liberia, Sierra Leone, Guinea)
and for any contact with someone who has travelled to one of those countries. If you get a yes to either of those questions immediately isolate the patient. Immediately notify the CDC. They will send a team to the hospital within 6 hours. Don PPE before initiating any further evaluation or treatment for the patient. Limit the number of healthcare workers coming in contact with the patient.

*CDC Screening Protocol
Precautions for healthcare workers caring for patients with suspected ebola infections require protection against contact and droplet exposure. Ebola is not thought to be airborne or aerosolized. Intubation/bipap/mechanical ventilation may have risks of aerosolization of the virus.
Patients who are ill with Ebola have extremely high levels of viremia in comparison to patients with HIV or hepatitis. This explains the infectivity of body fluids from patients sick with Ebola.
#2 Message: Meticulous donning and doffing of PPE is critical to avoiding healthcare worker exposure to the Ebola virus. This has to be a 2 person process that follows a check list every time.
The process of donning and doffing PPE was demonstrated by our advanced practice nurses. They are posting a video on the Advocate Website.