Conference Notes 11-12-2014
Knight/Gupta Oral Boards
Case 1. 28yo female, 38 weeks pregnant. She is complaining of shortness of breath with exertion. She also notes lower extremity edema. Pulse ox is 88% on RA. Lung exam demonstrates bi basilar crackles. CXR shows cardiomegaly and pulmonary edema. To complicate the situation, the patient is intent on signing out AMA. Diagnosis is peri-partum cardiomyopathy. Critical actions: Monitor fetus, treat CHF with O2 and diuresis and consult cardiology, consider preeclampsia. Convince the patient to stay in the hospital. Elise comment: You can’t keep this patient against her will. You can’t forcibly restrain her. If she has decisional capacity she will have to eventually be allowed to leave. This is a high risk situation.
Case 2. 9yo male with left elbow injury. Patient fell from a slide at school. Patient has swelling of left elbow/forearm region. Xray shows a montagia fracture. Critical actions: manage pain, diagnose montaggia fracture, discuss timing of surgery with orthopedics.
*montaggia fracture (fx of prox third of ulna and dislocation of radial head) Note that radial head does not line up with capitellum
Girzadas comment: The key to montaggia and galeazzi fractures are that they need ORIF. If you are not clear to the orthopedist when taking the oral boards as to the diagnosis, they will tell you to splint the patient and have her follow up. This will cause you to fail the case.
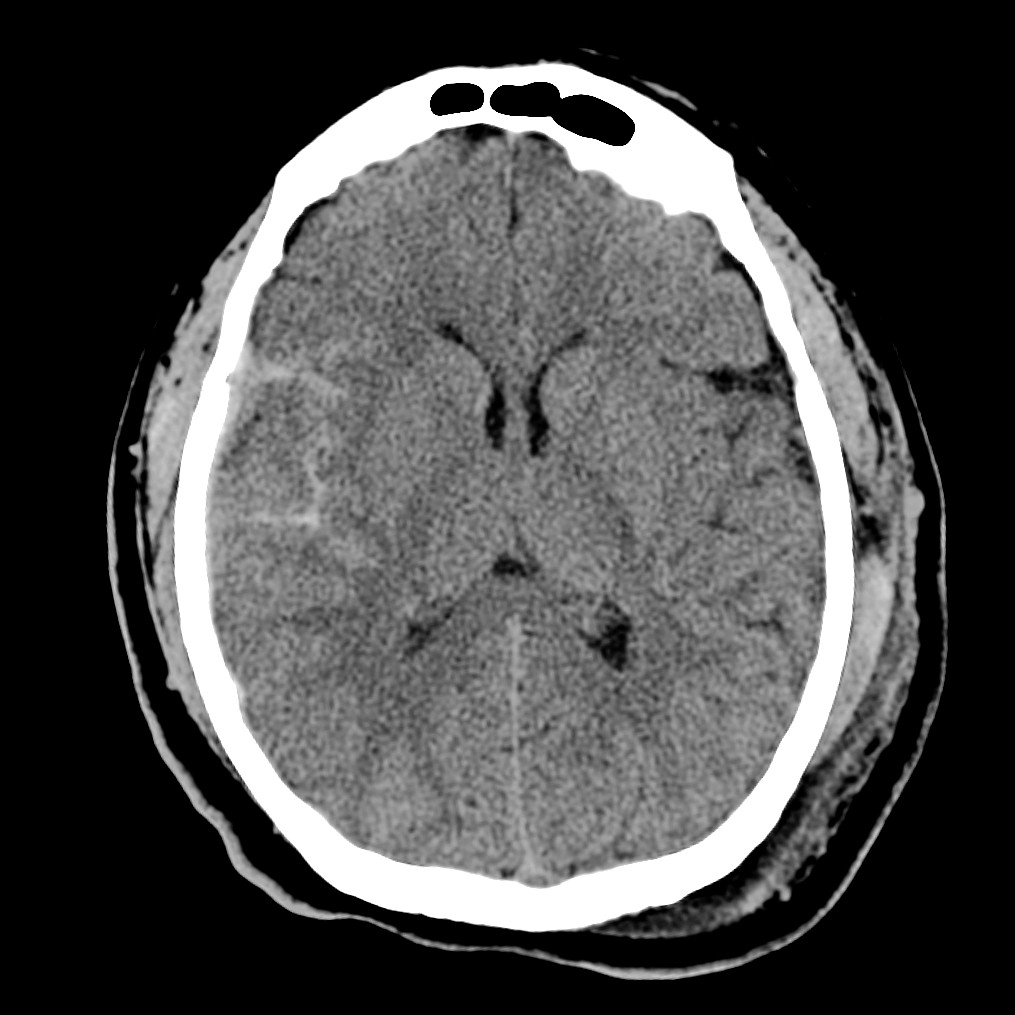
Case 3. 27 yo female presents with vomiting and diarrhea after eating at a restaurant. HR-124, BP=129/88. Rectal temp is 37.1C. On further history, patient also notes a headache and photophobia. Patient has neck stiffness on exam. CT head shows SAH.
*SAH
Elise comment: Don’t get sucked into the diagnosis of gastroenteritis based on the history of vomiting and diarrhea obtained in triage. Think through other differential diagnoses. Don’t write gastroenteritis as the diagnosis on the chart. Better to say vomiting and diarrhea. With careful history this patient did not have diarrhea actually. She actually had headache and vomiting and the triage note was misleading.
Harwood comment: With the oral boards you have to move through the cases quickly. Use the images /stimuli to key you into the diagnosis.
Parker Traumatic Brain Injury
35 yo male found down in an alley. Airway was OK. GCS was 10. Patient had frontal hematomas. GSW to the occiput. Presumed mechanism was that patient was shot in the back of the head and fell forward. CT showed cerebellar bleed and edema due to the GSW. Patient also had midline shift on higher cuts on the CT. Incidentally, patient had a retrobulbar hematoma of the left eye. Patient was intubated and taken to the OR for decompression. Patient deteriorated in the ICU and eventually was pronounced brain dead.
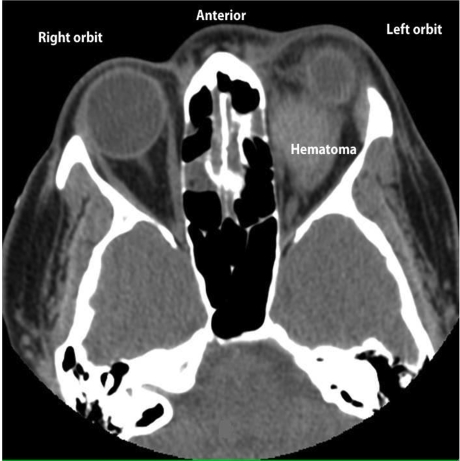
*retrobulbar hematoma
ED priorities for the management of TBI: Prevent secondary insult to the brain by avoiding hypotension and hypoxia. A single occurrence of hypoxia or hypotension results in a 150% increase in mortality. So, intubate early. Use fluids and pressors as needed to maintain SBP. Mannitol can be effective if the patient is at risk of herniation. Prophylactic hypothermia is not currently recommended. 20% of patients with severe TBI will have a dvt/pe. Use SCD’s and consider LMWH to prevent dvt/pe. If the ICP >20 treatment to lower ICP should be initiated. Keep cerebral perfusion pressures between 50-70. Prophylactic anticonvulsants can decrease the rate of seizures in the first 7 days. It does not help decrease the rate of seizures after 7 days. Hyperventilation can be used cautiously for patients with significantly elevated ICP and at risk of herniation. Steroids are contraindicated for TBI. This is the one level 1 recommendation for TBI, no steroids.
Braden recommended the Brain Trauma Foundation guidelines for management of head trauma. https://www.braintrauma.org/coma-guidelines/searchable-guidelines/
When consulting neurosurgery for TBI, be able to relay the history of the injury, any use of anticoagulants, CT findings, mental status, and the trajectory of the patient’s mental status. The neurosurgeon needs this info to make a decision of whether to come to the hospital or not.
Elise comment: Be alert to new evidence coming out about therapeutic hypothermia for TBI. There are some multi-center studies that will be coming out soon and possibly support new recommendations for the management for traumatic brain injuries.
Christine comment: Remember that Coumadin isn’t the only blood thinner that patients can be on these days. You may have to carefully ask patients about what medications they are on to not miss other blood thinners like rivaroxaban or clopidogrel for example.
Difficult Conversations Workshop
Michigan model: Medical Center Physicians/Administrators apologize to the patient and their families and explore how things went wrong. They will explain to the injured parties what happened. They vigorously defend the case when they feel they are right. Litigation is viewed as a last resort. Michigan has differences in malpractice law from Illinois that may limit implementation here.
We broke out in to small group simulations covering:
Raising a concern with family for pediatric abuse
Death notification of an adult
Discussion of end of life choices for critically ill/poor prognosis patient
Disclosure of procedural complications
Disclosure of medical error
Death notification of child
General guidelines:
Meet with family as soon as possible.
Have the discussion in an area that is quiet and private.
Optimize your appearance prior to meeting with family (clean scrubs, lab coat).
Have plan in your head and take time to prepare what you are going to say before you get in the room.
Ask the family what they know and what their understanding of the situation is before you give information.
Provide the information as clearly as possible. If the patient died, you have to use the words dead or died.
There is controversy about offering an apology.
Give the family time to express their thoughts/feelings.
Express compassion for them. Offer support going forward.
Answer any questions.
Provide guidance on next steps.