Conference Notes 5-21-2014
Ireland Patient Satisfaction
People don’t cut you slack when comparing service. They know if it is good or bad. They will compare their experience in the ED with their experience at Disney or ordering from Zappos.
Who gets to decide how the experience was? Not the doc or the nurse but the patient.
Customer service is a moving target. Each year the bar gets moved higher.
75% of your workday involves work. Why not make it a positive experience. Work on things you can change: interactions with patients, co-workers, your attitude.
Everything is driven by culture. You have to develop a great culture to be great. You can design culture to be great.
Very effective organizations like Walmart and Walgreens are now our competition in the healthcare market. If we can’t get service right, we will be “eaten alive” by these big corporations. Culture is “the way we do things around here” Culture optimally is designed and intentional to get the results you want. As an example of culture by design, Dr. Ireland’s group story-boarded out what the perfect patient experience would be.
Great service is delivered by a conscious design of people, place, and process.
Patients can’t assess technical quality of health care. All they can assess is our service and if they like us.
Quality service=Exceeding expectations by paying attention to detail, layers of detail. Treat patients like they are quests in your home.
Doctors miss 90% of empathy cues when dealing with patients.
The main commodity of the 21st century is time. We gotta understand that to be successful. People value their time most of all.
Saying thank you to people is critical. Saying “Thank you” is the #1 way staff want to get positive feedback.
We judge ourselves based on our intentions but we judge others by their actions. We gotta stop doing that. We gotta judge ourselves by our actions.
68% of customers leave a company or patients leave a practice based on a negative or indifferent employee attitude. It is the #1 reason people seek another provider.
There needs to be 40 positive customer experiences to counter-balance a single negative customer experience.
What do customers AND employees want: Treat me special, treat me as an individual, treat me with respect, educate and develop me.
ARE=Appreciate, respect, encourage employees and customers.
Everything speaks to the customer. If a customer goes to a great restaurant and the bathroom is disgusting, that affects strongly the customer’s assessment of your restaurant.
Great systems deliver great service. Foster continual improvement, engage everyone, make it hassle free, Ask patients, ask patients, ask patients what would iprove their experience. Ask staff, Ask staff, Ask staff what would improve their experience. Guide patients through the experience.
There are many benefits of patient satisfaction: increased patient compliance, decreased malpractice risk, more fun, increased revenue. Docs gotta be careful because we will have yelp and healthgrade reviews of us on the internet.
Service Profit Chain:The most important part of the chain is internal service quality (how employees treat eachother) Internal service quality leads to employee satisfaction and employee retention and employee productivity. These all lead to external service quality which leads to customer satisfaction, customer loyalty and finally revenue growth.
*Service Profit Chain (google image)
We have medical knowledge that we learned in med school and residency. But the patient’s perspective depends on how we deliver this knowledge. We don’t get much training on how we deliver the knowledge we have.
Some good reads to follow up this lecture: “How to make people like you in 90 secs or less. “ “Hug your customers.” “What got you here, won’t get you there” “Creating Magic”
Tekwani Study Guide GI
Spontaneous bacterial peritonitis= Peritoneal fluid cell count >1000 or PMN’s>250. Treat with IV Cefotaxime or in penicillin allergic patients you can use levofloxacin. Common pathogens are e coli, strep, and klebsiella.
Acute Alcoholic Hepatitis: AST/ALT ratio >2, hepatomegaly, possibly low grade fever.
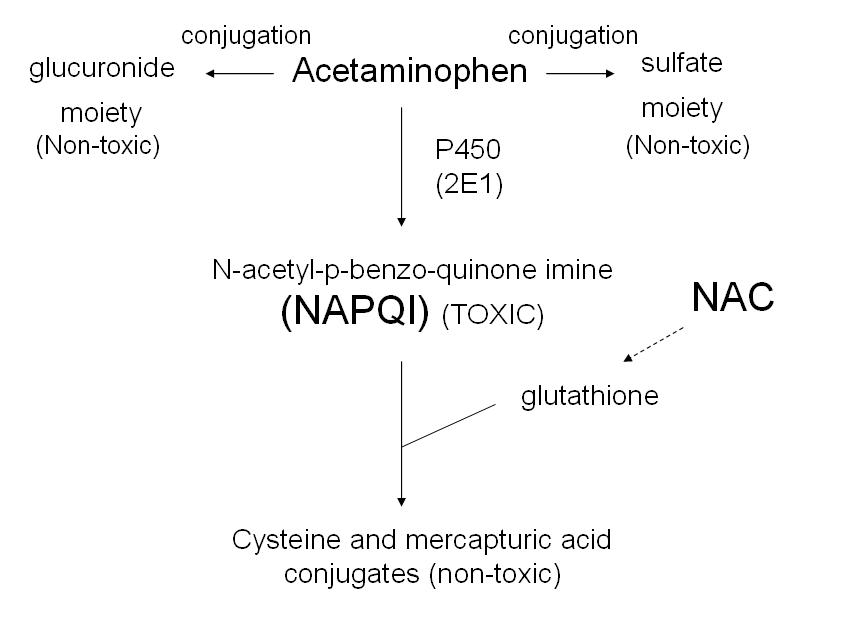
The most common cause of acute liver failure: acetaminophen. Hepatitis B is the most common viral cause of liver failure.
Anal fissure is almost always located in posterior midline. If fissure is in another location you have to consider crohn’s, syphilis, TB, HIV, cancer, or FB insertion.
Most common complication of cirrhosis: ascites.
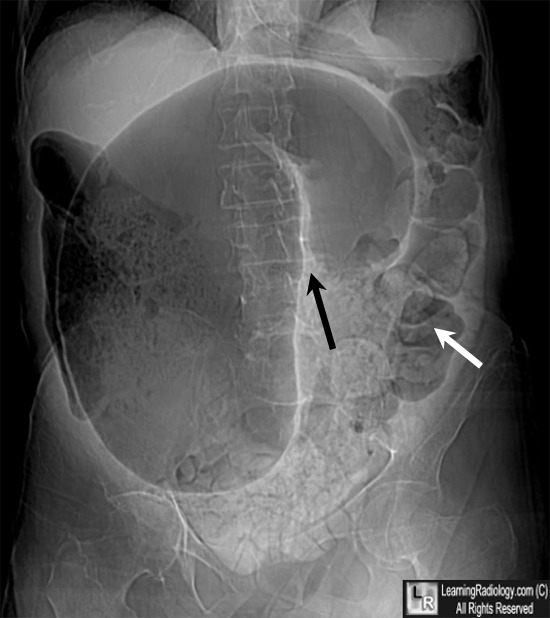
Sigmoid volvulus is more common than cecal volvulus. Sigmoid volvulus is seen in elderly bedridden patients. It is reduced endoscopically. Cecal volvulus is seen in marathon runners. Cecal volvulus is treated with surgery. Cecal volvulus on xray shows dilated bowel that extends up into left upper quadrant and sigmoid volvulus shows dilated bowel to right upper quadrant. Girzadas comment: I think about these volvulus’ as twisting to the opposite side of the abdomen with the cecum going to the left and the sigmoid going to the right when they develop volvulus.
*Cecal Volvulus (google image)
*Sigmoid volvulus (google image)
Toxic megacolon is treated with IV fluids, antibiotics, and corticosteroids. Toxic megacolon is more common in Ulcerative Colitis than Crohn’s.
Bowel rest for inflammatory bowel disease has not been shown to be useful.
The most common complication of diverticulosis is diverticulitis.
Pregnant women infected with Hepatitis E are more prone to fulminant liver failure. Hepatitis has nastier potential than hepatitis A with immunocompromised and pregnant patients at higher risk for chronic and fulminant hepatitis. Hepatitis E is the most common cause of hepatitis world-wide. Hepatitis A does not cause liver failure.
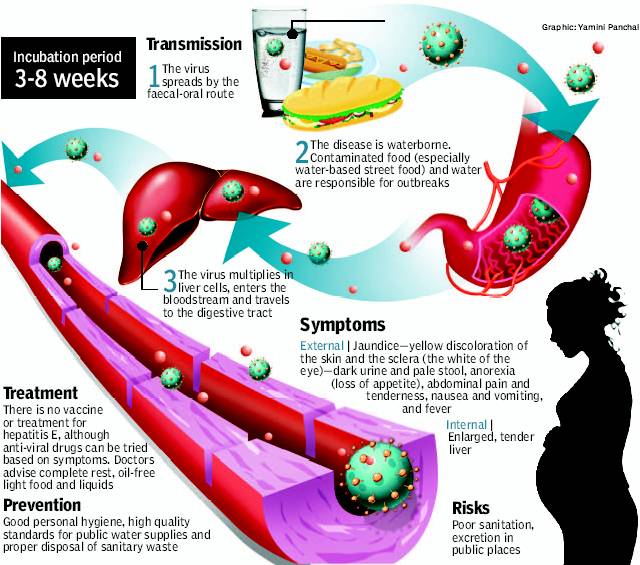
Hepatitis E (google image)
Most common cause of large bowel obstruction is neoplasm. #2 is diverticulitis. #3 is volvulus.
Most common cause of massive lower GI bleeding: diverticulosis
Lipase is more specific than amylase for diagnosing pancreatitis. Lipase and amylase have similar sensitivities for diagnosing pancreatitis.
Perianal complications are more common in crohn’s disease than in UC.
Erythema nodosum is more common in crohn's disease but can be related to either crohn's or UC.
Charcot’s triad for acute cholangitis: fever RUQ pain, and jaundice
Reynold’s pentad for acute cholangitis: fever, RUQ pain, jaundice, altered mental status, and hypotension. Most appropriate management of acut cholangitis is ERCP. IV fuids and broad spectrum antibiotics.
Undercooked shellfish has potential to transmit Hepatitis A.
Best treatment for uncomplicated diverticulitis: oral antibiotics
Complicated diverticulitis: phlegmon, abscess, stricture, obstruction, fistula, or perforation.
In acetaminophen overdose the normal liver pathways of glucuronidation and sulfation are overloaded and acetaminophen is metabolized by the P450 system to toxic NAPQI
*Metabolism of Acetaminophen Overdose
If you see HBeAG that means active infection of Hepatitis B.
*Hepatitis B serology
Girzadas comment: There can be confusion between HBeAG which is the active infection of HepB and Hepatitis E which is transmitted by the fecal oral route similar to Hep A.
The delta virus can only exist with Hepatitis B.
If patient has conjugated hyperbilirubinemia there is a post-liver obstructive process like sclerosing cholangitis.
Most common cause of anal fistula: intersphincteric abscess. This abscess is due to an infection of an obstructed anal gland.
CT scanning in first trimester of pregnancy doubles the infant’s childhood risk of cancer. However, in absolute numbers, the risk is still low.
Acute radiation protocolitis: diarrhea, rectal pain, tenesmus, abdominal pain. Treat with analgesics and sucralfate.
Katiyar Am I Really Too Slow?
RVU compensation was developed in the 1980’s. RVU is based on time, skill, training, and intensity. RVU=work produced. An RVU is assigned to every CPT code based on work, practice expense, and professional liability. RVU values increase proportionally with increasing EM code. Levels 4,5,critical care cases have the highest reimbursement. A level 4 chart brings in a $114. A level 5 chart brings in $168. A critical care chart brings in $217.
There are two common reimbursement models that utilize RVU’s.
Model 1. Eat what you kill: 100% RVU reimbursement to the physician.
Model 2. Piece of the Pie: Guaranteed base salary and a portion of your reimbursement based on RVU generation.
You can maximize your RVU’s by seeing patients as quickly as possible and charting promptly and accurately.
Charting: Chintan’s mnemonic is a made up word “FourTwoTenEight” or “Fortutenate”. This word helps you remember Four HPI elements. Two PMH elements (PMH/surgical history plus either Social or Family history), Ten ROS items, and eight PE items that will get you to a Level 5 chart.
Abhi gave examples of ER docs being fired for having low RVU productivity.
If you don’t document your work well, it severely affects your RVU production for a shift.
Top 5 Critical care misses (not billing for critical care when it is appropriate): agitated patients, tertiary care transfers, overdose management with antidote, hypoxia with O2 sat<87% and treatment of hyperkalemia with IV drugs. All STEMI’s are critical care. If the patient does not stay in the ED for the full 30 minutes you can still legitimately document critical care if you chart after the patient leaves the ED or you discuss with family or consultants after the patient leaves the ED.
Ways to increase RVU’s: document your interpretation and management of cardiac monitoring. Document pulse ox/peak flow. Document your procedures. Always measure the length of lacerations. Document layers, location, and if any foreign body or debris.
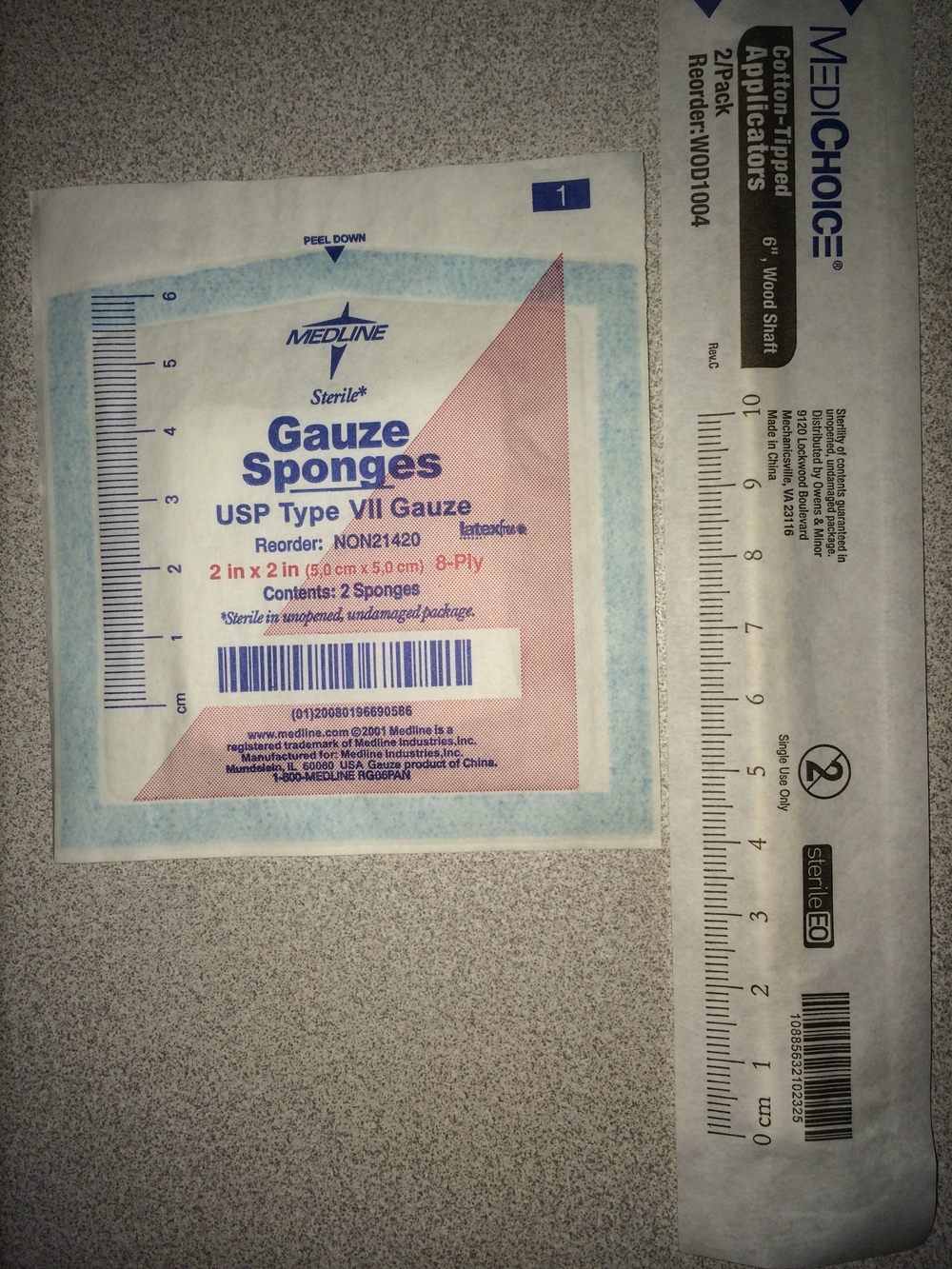
To measure laceration lengths, the paper wrapper of the cotton swab and 4X4 gauze have a ruler printed on them.
Packing abscesses increases the RVU for abscess management.
Documenting that you checked the neuro-vasc status of the patient after the tech has placed a splint increases your RVU. Sam comment: If you place your own splint you also increase your RVU’s.
Remember you are responsible for the accuracy of the bill no matter who does your billing.
Knight Safety Lecture
Surgery was consulted to repair a dog bite wound of the patient's ear. Patient was sedated prior to arrival of consultant. There was a patient handoff in the middle o this case. Consultant then notified ED that they were not going to be able to perform the procedure. We then had a patient sedated without a consultant to manage the problem.
We don’t have 24/7/365 coverage for peds plastics, peds neurology, peds facial fractures.
In the end, the ED physician repaired the wound in the ED and arranged plastics follow up for patient with plastic surgery.
Safety : Assure clear communication between hand off teams and consultants. Verify arrival times of consultants. Avoid sedating patient prior to arrival of consultant. Document all interactions with consultants.
Andrej and Elise comment: It is important to clearly convey the severity of wounds to consultants. A texted image of the wound is probably the best way.
Elise comment: Don’t sedate a patient prior to verifying that the consultant is in the ED to manage the problem. Start working on transferring the patient early in the ED course if you don’t have the required specialist on call. Harwood comment: It is important to communicate well with the family. Set up the situation that you are willing to repair the injury but that you are attempting to speak with the plastics specialist. Also inform the family that your child may need to be transferred.