Conference Notes 6-4-2014
Purnell/Patel Oral Boards
Case 1. 15 month old presents with choking/drooling/possible seizure. Temp is 37.7. No PMH and no meds. By the time the physician examines the patient the event has resolved. CXR shows coin lodged in esophagus at clavicles (thoracic inlet). Critical Actions: Consult GI for endoscopic removal of coin. Most coins (70%) get stuck at the thoracic inlet. 15% lodge in mid esophagus and 15% at lower esophageal sphincter.
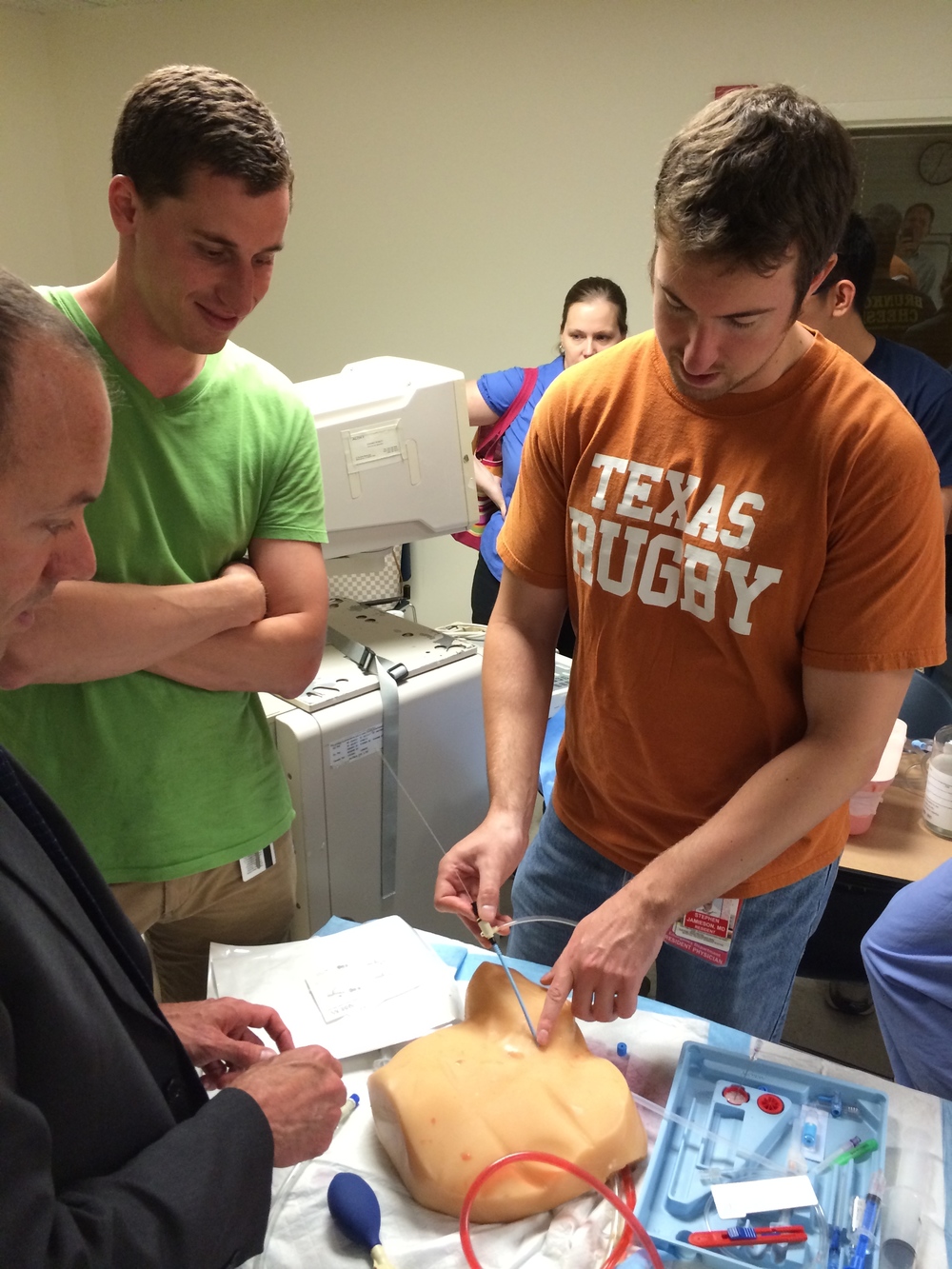
Case 2. 33 yo male presents with no pulse. Pt was electrocuted while working on power lines. Rhythm on monitor is ventricular fibrillation. Patient requires defibrillation. Labs show markedly elevated CK. Patient also has a compartment syndrome of the forearm. Critical Actions: Defibrillate, start amiodarone, give aggressive IV hydration for rhabdomyolysis, get emergent surgery consult for fasciotomy for compartment syndrome. Update Tdap. Cosnult Burn Center. Elise comment: Don’t say I want to shock the patient. You need to specifically say either “I am going to cardiovert the patient” or “I am going to defibrillate the patient”. Any time patient’s clinical status changes, be sure to re-evaluate the whole patient just as you would do in real practice. Be sure to differentiate between escharotomy and fasciotomy. Escharotomy is cutting through severely, circumferentially burned skin to relieve tissue compression. This patient had compartment syndrome for electrical burn and needed fasciotomy. Most likely mechanism of injury is heating of bone which has high electrical resistance and resultant injury to surrounding muscle compartments. Also, in the patient who suffered severe electrical injury consider other injuries such as C-Spine injury or head injury.

*Fasciotomy (google image)
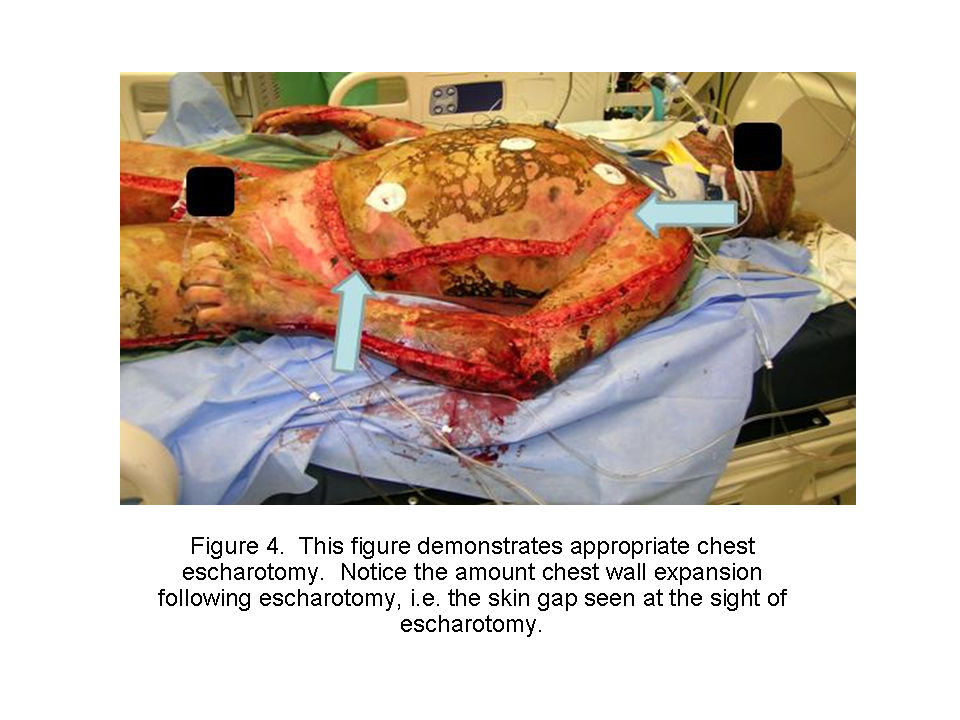
*Escharotomy (google image)
Case 3. 27yo female presents with generalized seizure. Patient also has fever/tachycardia/hypertension. Urine pregnancy test is negative. Patient was travelling through airport and developed seizure while in customs. Critical Actions: Initial Ativan terminates seizure. Patient was intubated for airway protection when her mental status did not clear and she had pooling secretions in her airway. Patient was found to be a drug packer. IV Ativan given again. IV phentolamine was also given for severe hypertension. Consult surgery for emergent laparotomy. Difference between packer and stuffer: Packers carefully wrap drugs to prevent spillage and put a large amount of these packages in their gut. Stuffers rapidly put un-packed drug in their mouth and swallow it to avoid arrest for drug possession by unexpected arrival of police.

*Drug Packer (google image)

*Drug packages removed from above patient (google image)
Maletich comment: If you are going to lap a patient should you be giving whole bowel irrigation? Elise comment: If patients are toxic from the drug they packed, you go to surgical mode and patient should get an emergent laparotomy. WBI is only for asymptomatic packers. Christine comment: Be aggressive with benzos in the management of cocaine toxicity. Elise comment: Any oral boards patients from the airport will likely be a tox case or an infectious disease case.
Harwood comments: patient 1 needs to get endoscopy, patient 2 needs to go to a Burn Center, patient 3 needs to go to OR. The choice of phentolamine for hypertension related to cocaine toxicity was excellent.
EM/PEDS Joint Conference Appendicitis
There still is a lot of controversy regarding the best management of appendicitis.
In a patient with high likelihood of appendicitis do you need imaging? Lobe response: If the diagnosis is clear cut I don’t need imaging. Other surgeons present felt ultrasound as the first imaging study was safe and indicated in most patients being evaluated for appendicitis.
Mary Ann Collins comment: In uncomplicated appendicitis we chose cefoxitin antibiotic coverage peri-operatively based on antibiograms for gram negative gut flora and anaerobes.
Lam comment: Approximately 50% of ultrasounds for pediatric appendicitis are non- diagnostic. Collins and Slidell comments: Radiology is working to decrease their rate of non-diagnostic ultrasounds. CT imaging does carry radiation risk. You can lower the dosage of radiation for CT’s in kids. This is protocolized for all kids getting an appendicitis CT study here at ACMC.
Lo comment: A non diagnostic U/S is not entirely unhelpful info. The fact that nothing was seen on the U/S does lower the risk of appendicitis.
Slidell comment: MRI for pediatric appendicitis works well. It may be something we will start doing in the near future. 2013 study of MRI for appendicitis showed 100% sensitivity and 96% specificity of MRI for appendicitis with no radiation exposure. This modality is probably useful only for teenagers due to the need for the patient to be very still.
In a patient with moderate probability for appendicitis: When the ultrasound is indeterminate, is there a role for serial exams instead of going to CT? Panel all agreed that serial exams have a role.
If U/S is read as negative, does that rule out appendicitis? Panel agreed yes it does.
If U/S is positive for appendicitis can the patient be treated with antibiotics instead of surgery? Surgeons’ comments: There is a limited role for antibiotics as definitive appendicitis management but we don’t have good criteria to select which patients will succeed with antibiotic management.
There was agreement that if there is a radiologic diagnosis of appendicitis and OR is planned for several hours later then starting IV antibiotics is indicated.
Harwood comment: Which antibiotic and when is the best option for uncomplicated appendicitis that is waiting to go to OR? Slidell and Collins response is the answer is not clear. Very muddy waters. Cefoxitin is a reasonable choice. Surgeons prefer that ED physicians start antibiotics in ED.
Slidell Un-Complicated Appendicitis
There is much variability both nationally and internationally regarding the management of appendicitis.
Atypical presentations occur in 50% of cases. The diagnosis is more difficult in kids less than 4 years old, females, and those with co-morbid illness.
There may be different types of appendicitis that have different courses of illness.
Most hospitals have a negative appendectomy rate from 0-17% median is about 2.5%.
Median range of ruptured appendicitis is 37%.
Median LOS for uncomplicated appendicitis is 1.8 days. Ruptured appendicitis patients stay for 5.2 days.
Laparoscopic surgery is the predominant approach for surgical management of appendicitis.
Risk factors for complicated appendicitis: poor healthcare access, children under 4 years old, co-morbid illness.
No increase in perforation rate or morbidity if surgery is delayed 12-24 hours. In general outcomes are better during day time compared to night time surgery.
Timing of surgery within 12-24 hours of presentation does not affect outcome or complication rate of appendicitis. There are studies showing that delaying surgery beyond 24 hours does increase perforation risk. Bill Schroeder comment: What is the start time for all these studies, onset of symptoms, time of presentation to ED, or time of radiologic diagnosis? Slidell response: It is not standardized in these studies. My take is that we should operate as soon as possible and 12-24 hours from ED presentation seems reasonable.
Children operated in the morning after overnight antibiotics had lower rate of abscess formation.
Antibiotics for appendicitis: Peri-operative antibiotics for 24 hours in un-complicated appendicitis. Perforated appendicitis gets about a week of antibiotics. Gangrenous appendicitis falls somewhere in-between. At ACMC we include gangrenous appendicitis in the perforated group and manage them with 7 days of antibiotics.
Treatment of appendicitis with antibiotics only has a success rate of about 70% vs. 97% success rate of surgery. (Cochrane review of mostly adults). 20-50% of patients treated with antibiotics alone will eventually need surgery for appendicitis within the next 12 months.
Small study of kids recently showed that 27 of 30 kids managed with antibiotics only had no problems by 6 moths.
Possible risks factors for failure of antibiotic therapy are: fecolith on imaging, duration of symptoms more than 24 hours, WBC>18, elevated CRP. There is a current multi-center study based at U of C assessing this issue.
Harwood comment: Kids managed with antibiotics will need imaging their whole life if they have abdominal pain. Also it has been shown that patients treated with antibiotics tend to have a higher incidence of chronic abdominal pain.
Some surgeons make the analogy that non-complicated appendicitis is essentially a version of diverticulitis. If you treat with antibiotics, it makes the surgery no longer an emergency. Appendectomy becomes semi-selective once antibiotic therapy has been initiated. This is not the concept that lay people have known previously. Harwood comment: The analogy is not perfect. You have one appendix and potentially hundreds of diverticuli. Diverticulitis has a high cure rate with antibiotics @99%. Appendicitis cure rates with antibiotics are @70%. There is a very low risk surgical procedure to treat appendicitis. Surgery for diverticulitis has higher risks and at times results in colostomy. So uncomplicated appendicitis has worse cure rates with antibiotics and lower risks associated with surgery than diverticulitis.
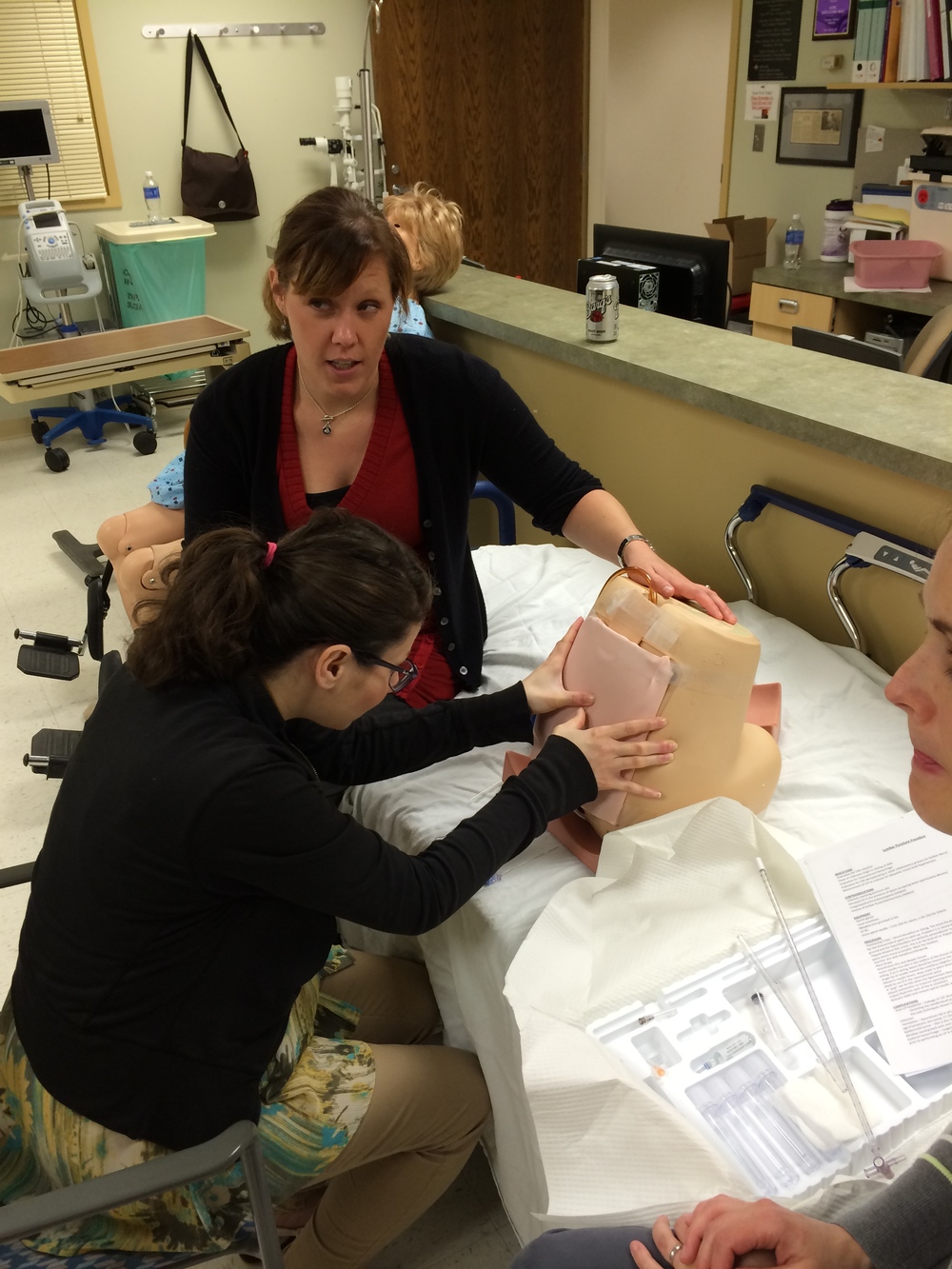
Advanced Procedure Lab