Conference Notes 1-7-2015
Remke/McKean Oral Boards
Case 1. 2 month old male presents with excessive crying. P 176 BP 72/48 RR 28 P/O 99%
Mom notes child has been eating less. Vomited once. Child is full term with no health problems. Exam shows normal male infant except that patient has a swollen/tender/erythematous scrotum. Ultrasound shows left sided inguinal hernia. Bilateral testes have adequate blood flow. Attempts at ED reduction were unsuccessful. Surgery was consulted. Teaching point: Do a complete physical exam on crying infants including the genital area. Males can have a hair tourniquet, paraphimosis, torsion, and hernia hiding under the diaper.
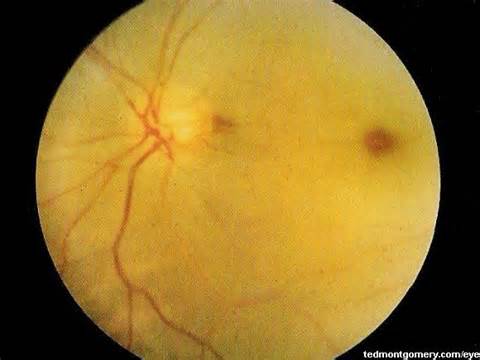
Case 2. 26 year old female with a chief complaint that she cannot see with her left eye. P 108, BP 138/78 RR 22 T 37. Patient has no headache or eye pain. No past medical history. There was a family history of an aunt with a “clot”. Patient was on oral contraceptive pills. CT and MRV imaging of the brain were normal. Fundocsopic exam shows
*Central Retinal Artery Occlusion
Treatment: There aren’t any evidence-based therapies. However you should try digital massage, timolol, and consult ophthalmology for anterior chamber paracentesis. Mannitol can also be given.
Teaching points: oral contraceptives can be a risk factor.
Case 3. 17yo male with knee injury during a football game. Vital signs are normal. Patient noted some transient deformity of his knee immediately following injury. The deformity spontaneously resolved. On exam, the knee is unstable. ABI’s of the injured lower extremity are also borderline abnormal. Plain x-rays of the injured knee show no abnormality. CTA of the injured extremity shows normal blood flow.
Diagnosis was a knee dislocation with a peroneal nerve injury.
Teaching points: Knee dislocations can reduce prior to ED evaluation. If you identify any neurovascular deficit there is increased risk for other neuro-vascular injury. The main injury to evaluate for is popliteal artery injury.
Elise comments: You have to be able to differentiate between central retinal artery occlusion and central retinal vein occlusion. Once you identify either, you need to move to treat that disease. Further testing is not going to be fruitful.
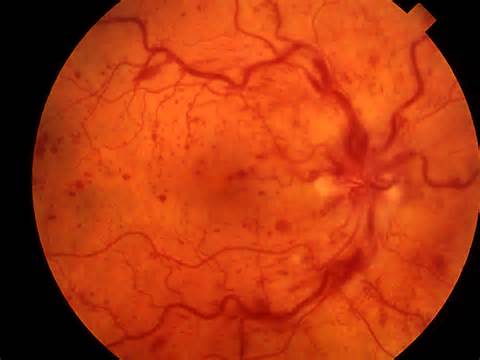
*Central retinal Vein occlusion
Carlson Critical Care Toxicology Updates
Poisoned patients spend less time in the ICU, have lower mortality, and have less mechanical ventilation days when compared to all other ICU patients.
Which toxicology patients should be intubated?
Tox patients don’t necessarily follow the trauma-based rule of GCS < 8 = intubate. One Dutch study showed the only 20% of toxicology patients with GCS 3-8 required intubation. If you have to sedate a tox patient to intubate them/keep them intubated consider that maybe you don’t need to intubate them in the first place. When making an intubation decision, you need to consider the duration of the toxin. Also consider if there are any reversal agents for the suspected toxin.
Pulse oximetry can be a useful tool to monitor hypoventilation. With no supplemental oxygen, the pulse ox will show a drop in O2 saturation that pretty predictably corresponds to a rise in a PCO2. If you give supplemental O2, this will blunt the drop in O2 saturation and you can miss hypoventilation. We then had a lively debate about using supplemental O2 for procedural sedation. The pro side: you potentially protect against hypoxemia. The con: It may mask hypoventilation. The consensus: Give supplemental O2 and use capnometry to pick up hypoventilation.
Hypercapneic respiratory failure is probably the most common reason for intubation of a toxicology patient. Etoh, benzo’s, opioids, and other sedative hypnotics are common drugs causing hypercapneic respiratory failure.
Hypoxic respiratory failure is less common in toxicology patients but can develop from pulmonary edema or aspiration.
BiPap is less useful for tox patients. Predictors for Bipap failure include weak cough reflex, excessive secretions, hypercapnea, and agitation. All of these are common in tox patients. Vomiting is another big problem with bipap for tox patients. The risk of aspiration is very high. Bottom line: no role for bipap in a tox patient.
Ventilator settings recommended for the toxicology patient: Assist control, tidal volume of 6-8cc/kg of IBW (use 8cc/kg if the patient is acidotic/salicylate poisoned), If the patient is acidotic and tachypneic prior to intubation, the respiratory rate you set on the ventilator should equal the patient’s spontaneous respiratory rate prior to intubation. If the patient has an acid-base critical poisoning they need higher tidal volumes. Critical acid base poisonings that require higher respiratory rate and tidal volume vent settings include salicylate, barbiturate, and TCA poisoning, and any patient with a critical ph. If these patients are hypoventilated their acid-base status will rapidly decompensate.
The first hour after intubation is the time when the tox patient will crump.
In all intubated patients (both tox and non-tox) 25% will have hyotension and 4% will have cardiac arrest in the first hour after intubation. In tox patients, these numbers are even worse.
Barounis comment: THAM is buffer that can be given intravenously as a weight-based drug to counter acidosis. It works like bicarb but unlike bicarb does not get metabolized to CO2 that can cross the blood brain barrier and increase CNS acidosis.
Barounis ECMO in Critically Ill Adults
Case: 19yo female post-partum day 2. Pt had post epidural headaches and failed blood patches. Patient developed status seizures. Patient was placed on high dose propofol. Patient developed propofol infusion syndrome.
Propofol infusion syndrome:
Propofol infusion syndrome (PRIS) is a rare syndrome which affects patients undergoing long-term treatment with high doses of the anaesthetic and sedative drug propofol. It can lead to cardiac failure, rhabdomyolysis, metabolic acidosis, and renal failure, and is often fatal.[1][2][3] Hyperkalemia, hypertriglyceridemia, and hepatomegaly, proposed to be caused by either "a direct mitochondrial respiratory chain inhibition or impaired mitochondrial fatty acid metabolism" [4] are also key features. It is associated with high doses and long-term use of propofol (> 4 mg/kg/h for more than 24 hours). It occurs more commonly in children, and critically ill patients receiving catecholamines and glucocorticoids are at high risk. Treatment is supportive. Early recognition of the syndrome and discontinuation of the propofol infusion reduces morbidity and mortality. (Wikipedia)

*Propofol infusion syndrome
She develops persistent hyperkalemia and persistent ventricular tachycardia. Echo shows severe global hypokinesis. Patient arrests. She is placed on ECMO and dialysis. Over several days, the patient’s renal function improves and her cardiac function improved. She eventually was discharged with full neurologic function and ability to nurse and care for her child.
ECMO is a bridge. It does not treat any disease It buys you time to treat a patient.
VA- Full ECMO: Blood is drained from vena cava and returned to a femoral artery catheter. In between the EMCO circuit oxygenates and pumps the blood. There are many options for placing the circuit catheters. The most common catheter placement is the venous catheter placed in the femoral vein up to the right atrium. The arterial catheter is placed in the femoral artery.
With the patient on ECMO the medical team manages the O2 saturation, CO2 removal, MAP, hematocrit, and temperature. MAP is kept around 65. Hypothermia is induced to increase SVR and improve MAP. Pressors are also used to maintain blood pressure. The ECMO pumps do not provide pulsatile flow so the patients have no pulses. Patients on ECMO are heparinized and at high risk for bleeding.
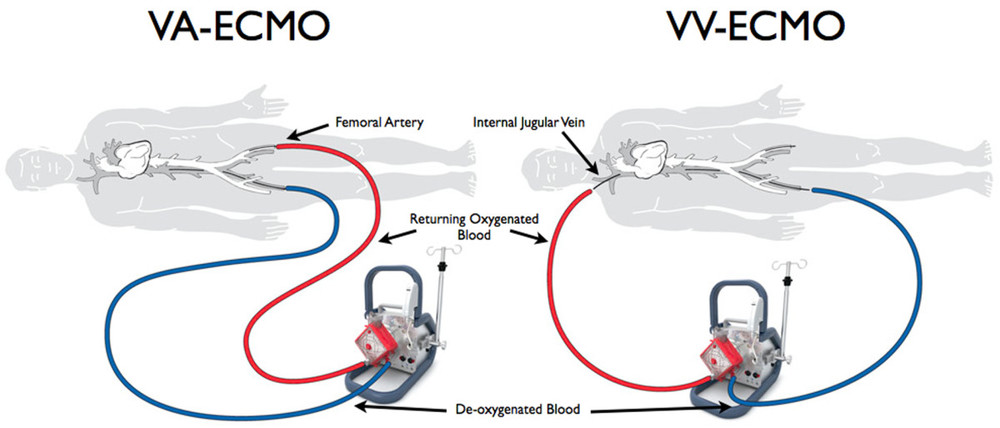
ECMO Diagrams
5% risk of intracranial hemorrhage with ECMO.
Dave then made the case for using ECMO in the ED. ACLS has a low rate of intact neurologic survival. There are multiple studies showing that patients who underwent prolonged CPR (30-60+ min) and then reeived ECMO have a good chance of survival with full neurologic recovery. Dave specifically discussed a study looking at patients with VF/VT arrest who underwent CPR for 30 minutes. ECMO was initiated after 30 minutes of ACLS care. This study had a 54% percent survival rate of the ECMO patients in which all survivors had good enough neurologic function to live independently at home. There was a discussion about whether our healthcare system could support the costs of utilizing ECMO routinely in cardiac arrest patients.
HTET Devices in Human
Case: 50 yo female with tracheostomy tube presents in full arrest. It was difficult to bag-valve- ventilate patient due to missing inner cannula of tracheostomy. Another inner cannula was place in the tracheostomy tube and ventilation could be accomplished.
Tracheostomy tubes: measurement is based on inner diameter. A 4.0 Shiley has a 4mm inner cannula. When placing the tracheostomy tube, have the obturator in place. When the tracheostomy tube is properly positioned, remove the obturator and insert the inner cannula so that the patient can be ventilated.
Trach tubes should be changed out about every 3 months. The inner cannula should be taken out and cleaned every day.
Dislodgment, obstruction, infection, and bleeding are the most common complications of a tracheostomy tube. Blind replacement is ok >7 days post op. You can intubate orally if necessary as long as pt has not had total laryngectomy. If a patient can make some noise orally they likely have not had a total laryngectomy.
Obstruction can be improved with suction, saline irrigation, humidified air and remove/replacement of inner cannula. If patient is crashing, remove the tracheostomy tube and replace with another tracheostomy tube or endotracheal tube. Alternatively you can orally intubate if the patient has not had a total laryngectomy.
Bleeding: Minor bleeding can be controlled with pressure, packing, or cautery. Be alert to possibility of a sentinel bleed from a tracheo- innominate arterial fistula. This occurs between 2 days and 6 weeks after surgery. The bleeding develops from the innominate artery. Treat trachea-innominate bleeding by hyper-inflating the trach cuff in an attempt to tamponade the bleeding. If the patient does not have a total laryngectomy you can intubate the patient orally, remove the trach tube, and put your finger in the stoma and compress the innominate artery against the sternum.
*Compression of trachea-innominate bleeding
Elise comment: If a patient has any bleeding from tracheostomy site between 2 days and 6 weeks after surgery it is a trachea-innominate artery fistula until proven otherwise. Knowing the timing of the tracheostomy procedure is critical for making this diagnosis early. You need to admit/observe these patients and consult pulmonary or thoracic surgery.
Air dissection: Air can dissect from trach tube down into the pleural space. Treat with needle thoracostomy and chest tube.
Tracheal stenosis: This is a delayed complication. A fibrous scar causes a narrowed trachea. This can occur a few weeks after de-cannulation. Treat with head elevation, cool mist, racemic epi nebulizer and steroids.
G-tubes
Clogged: Treat with warm water flush. Coca cola works well to dissolve the clog.
Deterioration: Yeast implants into wall of feeding tube. Replace tube. Ethanol also can be used to sterilize the inner portion of the tube.
Dislodgement: Replace tube if the tube was placed more than 4 weeks ago. The tube tract should be developed by 4 weeks.
Faculty discussed G-tube replacement tips: Sedate with versed or fentanyl. Intranasal meds for kids work great. Urojet lidocaine can be used in adults to give some local anesthesia. Use increasing diameter dilators to dilate the stoma (cervical dilators, foley tubes, NG tubes). Get a gastrograffen KUB almost always to ensure proper tube placement. Harwood felt that if the tube passes easily in to a long term stoma tract and you get gastric contents back you most likely are safe but if you have any doubt at all get a gastrograffen x-ray to verify placement.
Peristomal leakage: loosen or tighten the external bolster, apply zinc oxide paste. Can discuss with GI consultant about using larger tube. The tube size is not a common factor causing peristomal leakage.