Conference Notes 5-20-2015
If you don't see images scroll to the bottom and click "view in browser"
Ryan Musculoskeletal Emergencies Study Guide
Spinal stenosis clues: patient walks in flexed forward position. Patient has lower extremitypain when walking. Patient has pain relief with sitting. No pain with sitting is the most specific historical clue. Spinal stenosis causes pain with exertion similar to vascular claudication. However, spinal stenosis pain does not resolve when the patient stops walking and remains standing. Vascular claudication should resolve when the patient stops walking and remains standing. Spinal stenosis pain won’t resolve until the patient can flex his hips by sitting , leaning forward, or squatting.
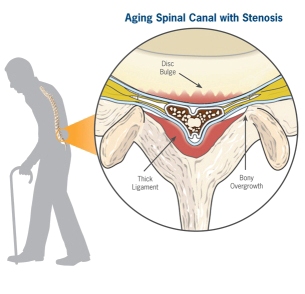
*Spinal stenosis
*Normal healthy spine
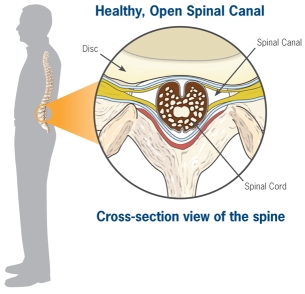
Adequate muscle relaxation is the most important factor in successful shoulder reduction
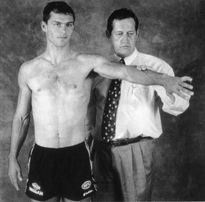
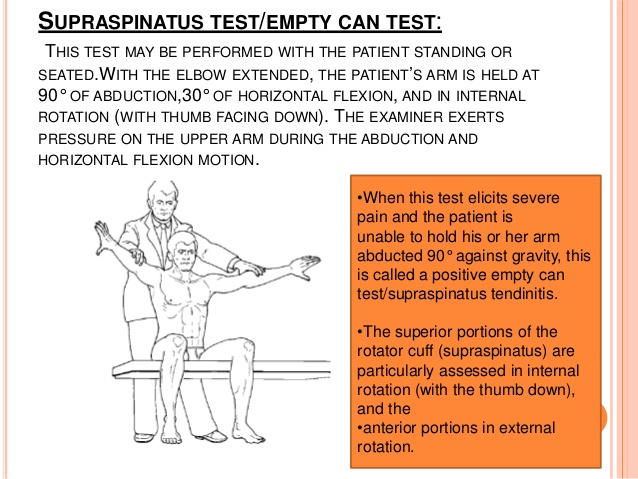
*Testing for supraspinatus Empty Beer Can Test (Jobe’s Test) Pain and weakness resisting downward pressure on the arm suggests a tear in the Supraspinatus Tendon
*Jobe's Test
Harwood comment: For knee injuries that swell immediately, there probably is a hemarthrosis. That is the only mechanism for a knee to swell immediately. For knees that swell up overnight that is more likely a reactive effusion.
Cauda Equina syndrome is associated with urinary retention.
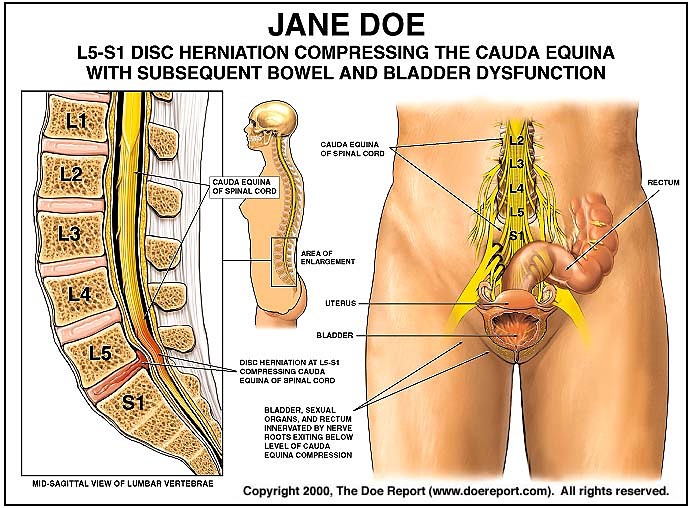
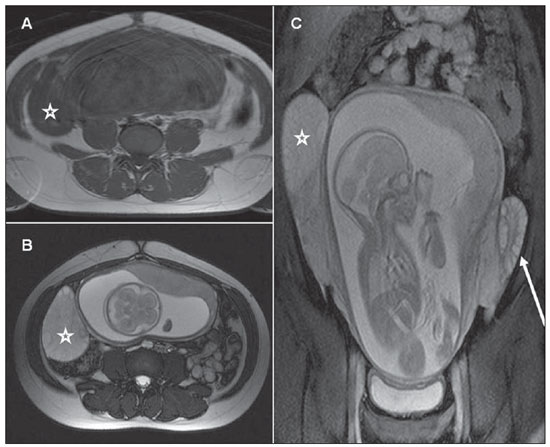
*Cauda equine syndrome
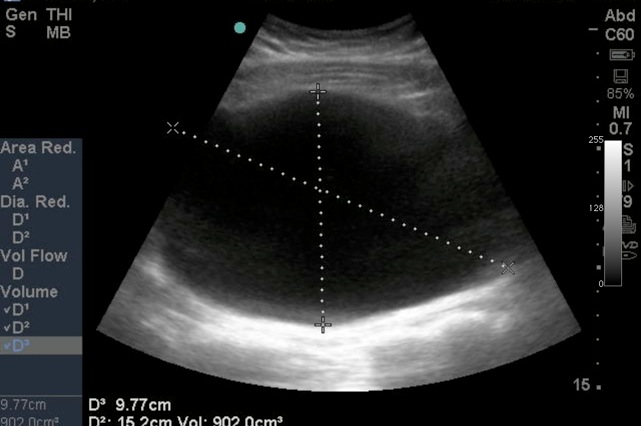
*U/S of urinary retention
Reimplantation of amputated digits is basically all about the thumb. Discusss with the hand surgeon prior to discarding any tissue. Keep the amputated finger wrapped in saline soaked gauze. Place the saline gauze-wrapped digit in a plastic bag and place the bag on ice. Keep the digit in a cooler that stays with the patient.
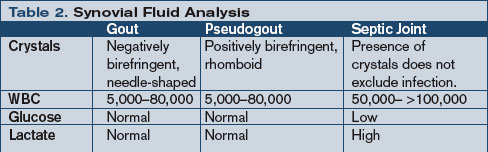
*Gout vs Septic Arthritis
Jeziorkowski Trauma to Cervical Spine
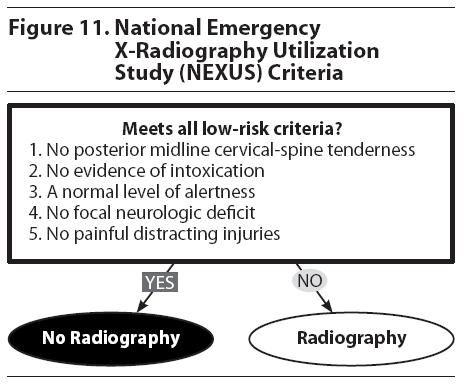
*Nexus C-spine Rule
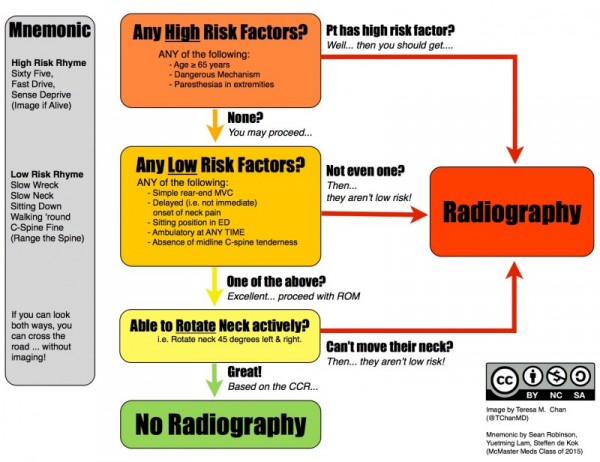
*Canadian C-Spine Rule
Elise feels the Canadian Cspine rule is superior to the Nexus rule based on it’s increased specificity. If the Canadian C-Spine rule indicates imaging, go to CT rather than plain films.
We also discussed the practice of placing an axial load on the patient’s head to check for tenderness. It was felt among the group that if you do the Canadian Cspine rule first with head turning prior to axial loading, it probably isn’t a dangerous practice to axial load, but it also is not useful. Axial loading is probably not a useful test for assessing the Cspine.
EAST recommends CT as the imaging method of choice for the Cspine. Plain films are only indicated for a young, non-obese, non-extremely muscular person with a low-risk mechanism of injury.
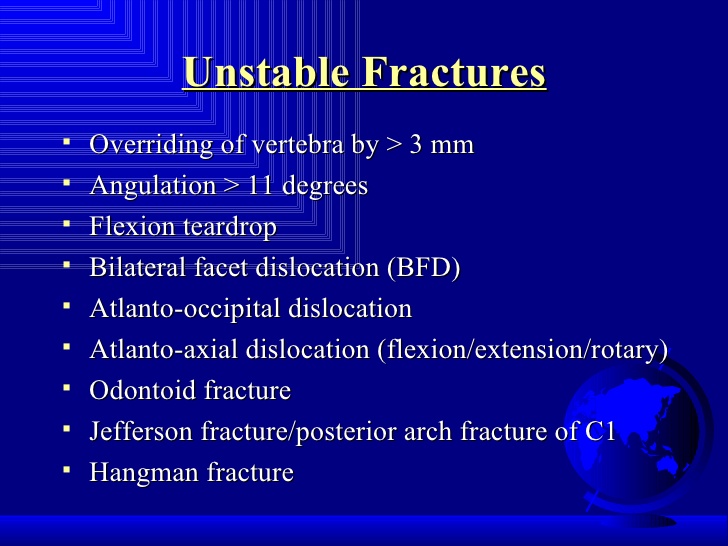
Chris discussed multiple unstable C-spine fractures
*Unstable Cspine Fractures
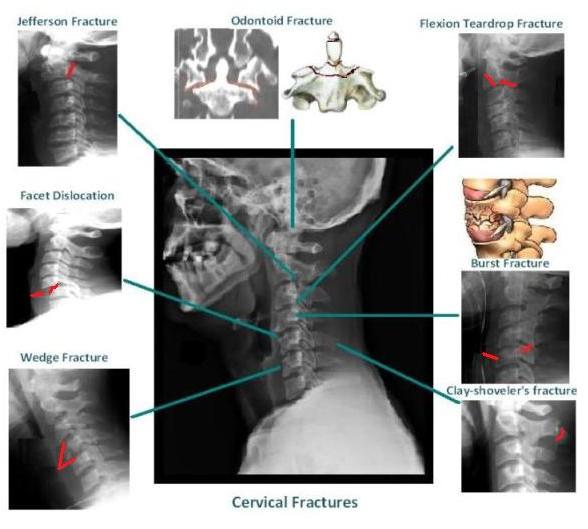
*Cspine Fractures
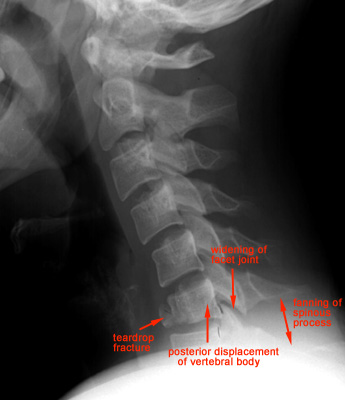
*Flexion Teardrop Fracture
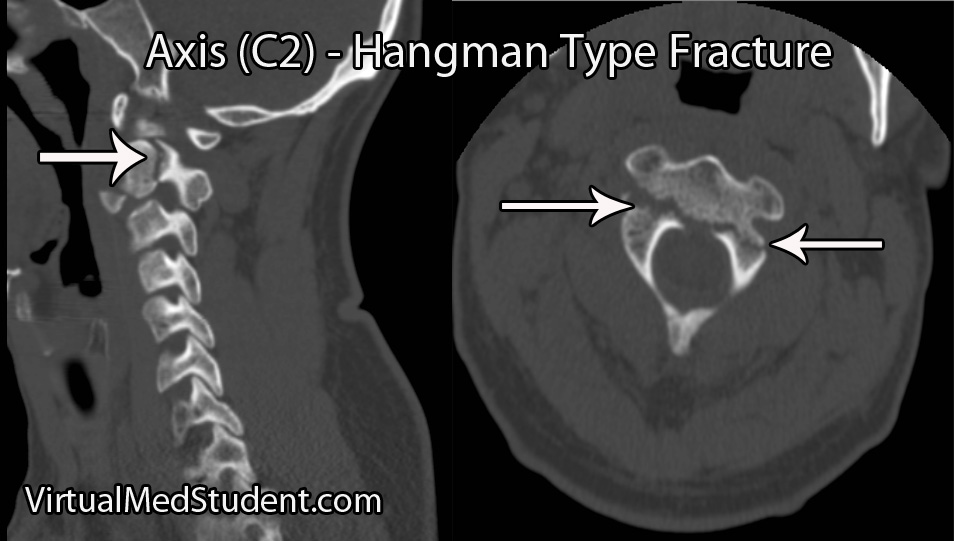
*Hangman’s Fracture
If CT Cspine is negative and patient has persistent severe pain or paresthesias you need to get an MRI. There is an entity called SCIWORA, which is a spinal cord injury without radiographic abnormality. This injury is usually a ligamentous tear. This injury can be best picked up by MRI. There was consensus among the attendings that flex-ex films are inferior to MRI for picking up ligamentous injury. Also all the attendings felt that patients who have some persistent midline posterior neck pain following a negative CT cspine but have low to moderate-risk mechanism and no neuro symptoms can go home without an MRI. It should be said that EAST still recommnends MRI for patients with persistent pain following negative CT. Most attendings felt it was unnecessary to MRI all these patients. A selective approach based on severity of pain, mechanism, and neuro symptoms seems reasonable.
EAST Guidelines recommend removal of c-collar after a negative CT scan of Cspine in a comatose patient. This is a brand new recommendation. There was some collective head scratching on this recommendation by the faculty. Most faculty felt they would still MRI this type of patient (head injured, comatose, in c-collar following negative c-spine CT)
Cash/Lovell Clinical Teaching
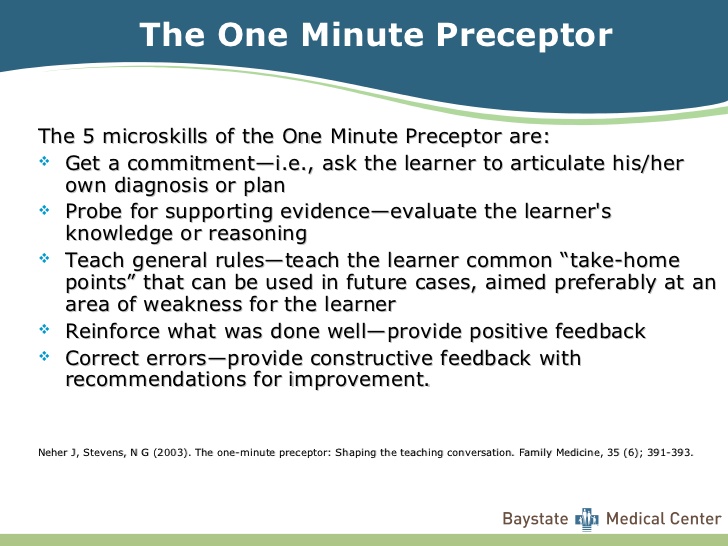
*One Minute Preceptor. Getting a learner to commit to a diagnosis they feel is most likely and defend that commitment is a key to this teaching method.
SPIT teaching method: Ask the learner to give a differential diagnosis in each of the following SPIT categories
Serious
Probable
Interesting
Treatable
This is an easy way to teach on almost every patient.
Create a motivating environment. Be an encouraging and supportive teacher. Give the learner specific feedback.
3 Step approach to teaching procedures
- Assess your learner’s skill level
- Teach Concepts. This includes repetition of the tasks of the procedure. Introducing a small bit of variation regarding how to perform the procedure helps with performance and long term retention of the skill. With more advanced learners’, focus on key portions of the procedure and discuss how to refine their technique. “What if” simulation scenarios a la Harwood asking you how would handle this procedure if the patient was pregnant or was a pediatric patient or had septic shock can improve the advanced student’s learning.
- Directed Feedback. Be specific in your analysis and suggestions to the learner.
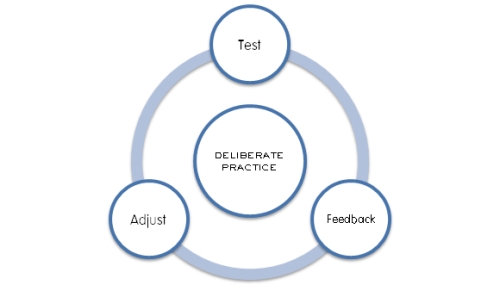
*Deliberate Practice
*Peyton’s 4 Step Model
*Elise then showed a video of how to make rabbit ears based on Peyton’s 4 Step Model. This skill was clearly mastered by multiple residents
Jamieson/Watts Oral Boards
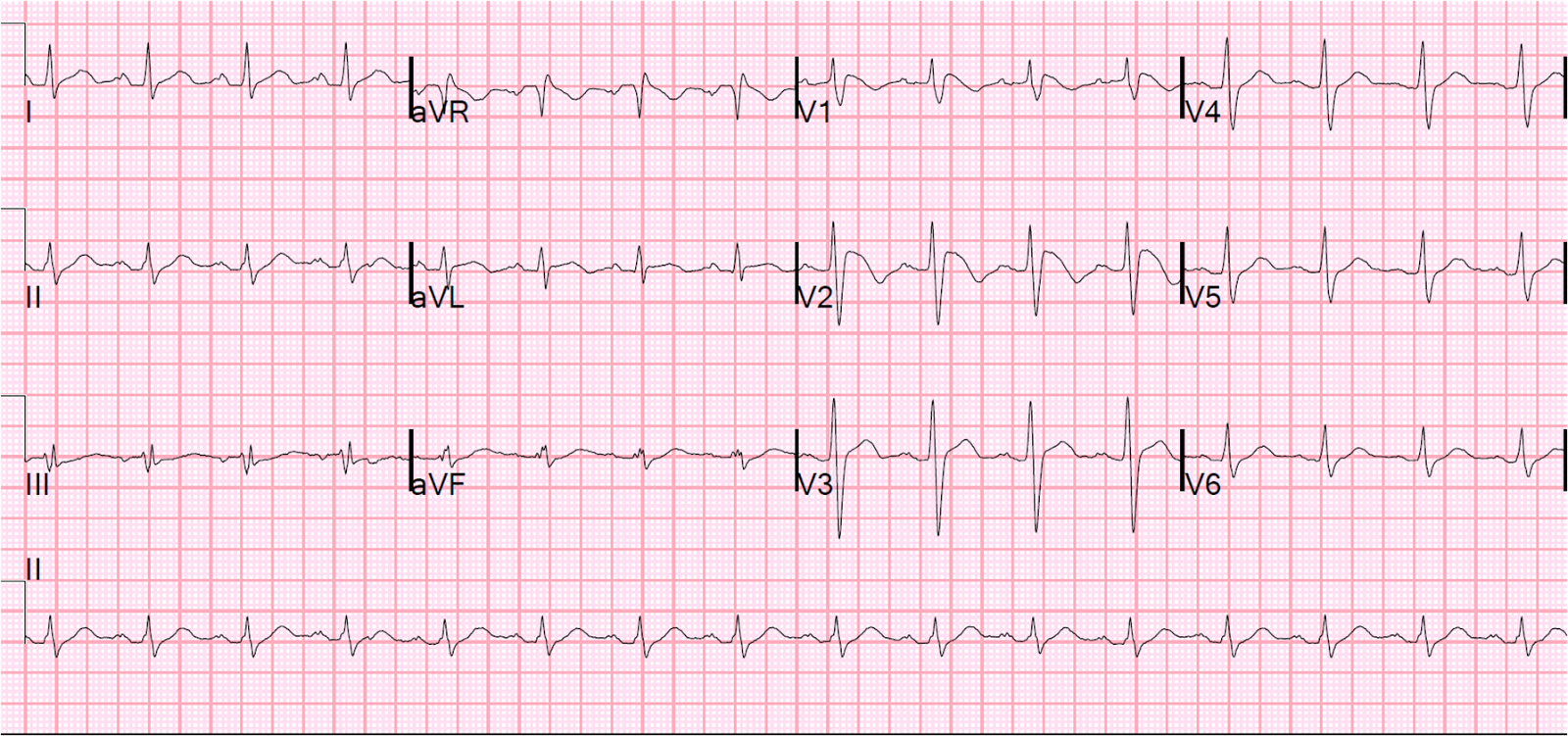
Case 1. Middle aged man presents with syncope while watching the Hawks game. Patient has history of cold symptoms for 2 days. Physical exam is unremarkable except for URI findings. EKG shows brugada changes.
*Brugada EKG V1-3 has RBBB pattern with ST elevation
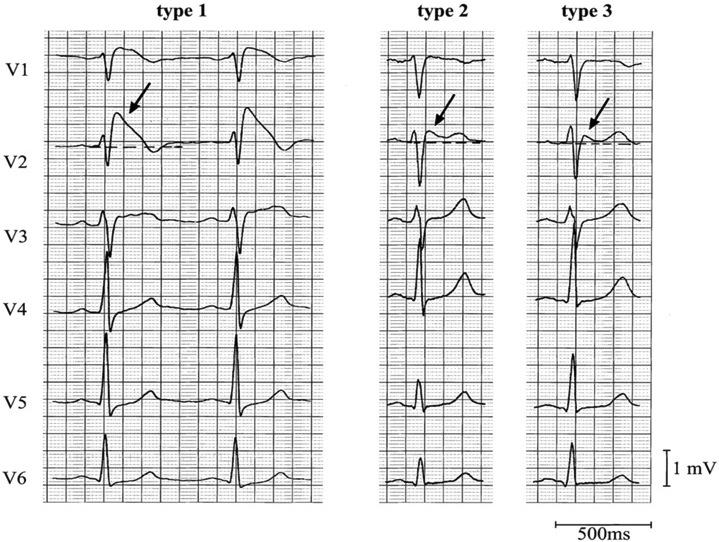
*Brugada types
Critical actions: Consult cardiology and admit for AICD placement.
Case 2. 16 yo female with hematemesis and syncope. Patient is tachycardic. Patient has history of autoimmune hepatitis. Patient develops massive hematemesis in the ED and becomes unresponsive. Critical actions: Patient is intubated to protect airway. 2 large bore IV’s, IV fluid resuscitation, IV PRBC transfusion. Protonix and Octreotide. Consult GI and admit to ICU. Ideal management includes NG tube and IV antibiotics (Rocephin or a Quinalone).
(International Journal of Hepatology 2011) Currently, it is recommended that short-term antibiotic prophylaxis, a measure that reduces bacterial infections [23], variceal rebleeding, and death [24], be used in every patient with cirrhosis admitted with gastrointestinal hemorrhage [20, 25, 26]. Different antibiotics have been used in different trials compared with placebo (Table 1, [27–30]). Bacterial infection is commonly associated with variceal hemorrhage and appears to be an independent risk factor for failure to control bleeding [31] and predicts both early rebleeding and death [32, 33]. The routine use of prophylactic broad-spectrum antibiotics has shown a marked improvement in outcome in acute variceal hemorrhage. Routine intravenous ceftriaxone or postendoscopic norfloxacin reduces rebleeding rates compared to on-demand antibiotics (Table 2) [24, 29, 34–36]. A Cochrane meta-analysis of antibiotic prophylaxis in cirrhotic patients with gastrointestinal bleeding involving 12 trials with 1241 patients evaluated antibiotic prophylaxis compared with placebo or no antibiotic prophylaxis. Antibiotic prophylaxis compared with no intervention or placebo was associated with beneficial effects on mortality (RR 0.79, 95% CI 0.63 to 0.98), mortality from bacterial infections (RR 0.43, 95% CI 0.19 to 0.97), bacterial infections (RR 0.36, 95% CI 0.27 to 0.49). They concluded that prophylactic antibiotic use in patients with cirrhosis and upper gastrointestinal bleeding significantly reduced bacterial infections, and seems to have reduced all-cause mortality, bacterial infection mortality, rebleeding events, and hospitalisation length. These benefits were observed independently of the type of antibiotic used [37, 38].
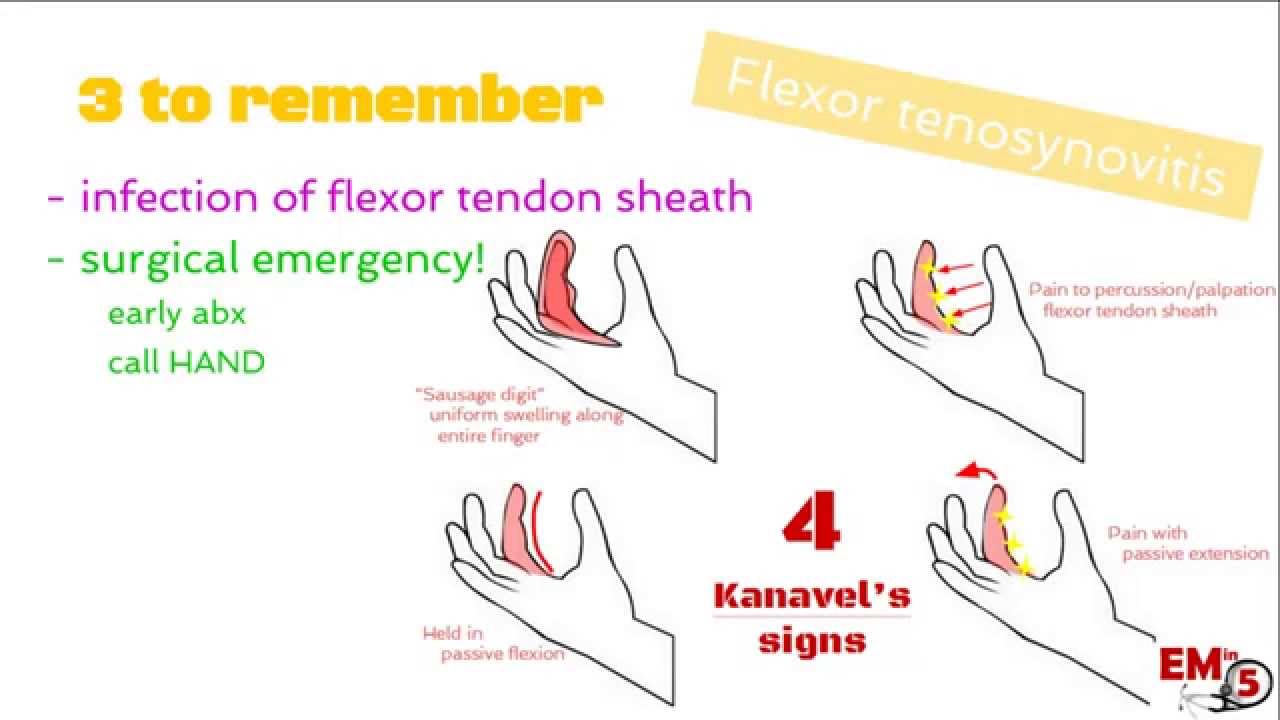
Case 3. 26 yo female with right index finger pain. Temp is 37.9C. Other vitals are normal. Patient has history of gardening and jabbed her right index finger on something sharp in the soil and suffered a laceration. Her tetanus status is up to date. Right hand demonstrates Knavel’s signs of flexor tenosynovitis on exam. Testing in the ED shows a positive pregnancy test. Patient also has a penicillin allergy. Critical actions: IV Clindamycin (Pregnancy Class B) to cover Staph, x-rays of right hand, Hand surgery consult for surgery.
*Knavel’s Signs of Flexor Tenosynovitis
Harwood comments: Great job telling the examiner what you know and thinking out loud. Get a rhythm strip on the first patient ASAP don’t wait for the EKG. You don’t need a CT scan of the head as part of a routine syncope work up.
Faculty felt that the tenosynovitis patient needed broad coverage including gram positive and gram negative coverage. Elise and Harwood felt a third generation cephalosporin plus/minus clindamycin would be reasonable. Girzadas felt clindamycin to cover MRSA was indicated.
This will give the alumni a laugh, but Girzadas advised doing a rectal exam on all syncope patients.
Lee 5 Slide Follow Up
35 yo female 28 weeks pregnant presents with abdominal pain. Patient was hospitalized at an outside hospital a week earlier for renal stones and ureteral stent placement. Vitals were normal/afebrile. On exam the patient had right lower quadrant and right flank tenderness. CBC showed a WBC of 15. Urine was negative for infection and positive for moderate blood. The initial thought was that the patient was having recurrent ureteral colic. Renal ultrasound here at ACMC showed mild hydronephrosis but no stones.
A pelvic ultrasound performed here at ACMC showed a right adnexal mass c/w right ovarian torsion. Laparotomy removed a necrosed dermoid tumor. It is conjectured that calcifications in the dermoid tumor that was adjacent to the kidney may possibly have complicated the ultrasound of the kidney performed at the outside hospital. This could have led to the initial diagnosis of nephrolithiasis and renal colic. We however did not have those images to review.
Pregnancy is associated with an increased risk of ovarian torsion. Torsion is most likely to occur between 10-17 weeks gestation. Torsion presents with pelvic pain, adnexal mass and nausea/vomiting.
The ovary moves upward toward the kidney as pregnancy progresses. This may make the diagnosis more difficult.
DDX for RLQ pain in a pregnant patient =ruptured cyst, ovarian torsion, appendicitis, tubo-varian abscess.
*MRI demonstrating right ovarian torsion with concurrent pregnancy. Notice how high that right ovary is.
Bamman 5 Slide Follow UP
3 yo male presents with fever and drooling Fully immunized. Child was cranky with chapped lips. There were no intra-oral ulcerations. The patient did not improve in the ED with magic mouthwash. And would not take a popsicle. Because this patient looked sicker than the usual kid with stomatitis and he did not have intra-oral ulcerations, a lateral soft tissue neck film was ordered.
Lateral soft tissue neck film showed possible epiglottitis.
Patient was taken to the OR for intubation. On laryngoscopy patient had epiglottitis. There was some tracheal pus. Tracheal cultures showed staph aureus. Patient was treated with Vancomycin and Zosyn and decadron. Patient recovered well after 3 days of intubation. Staph areus is becoming more common as an etiology of epiglottitis.

*Epiglotitis. This patient has a thumb sign and a vallecula sign. The vallecula sign is when the air column in the vallecula does not extend to the hyoid.