Holland/McKean Oral Boards
Case1. 55 yo diabetic male with right lower leg pain after getting a fish hook embedded in his right lower leg. Patient was fishing in the Gulf of Mexico. Xrays show SubQ Air.
*1 SubQ Air
Diagnosis was necrotizing fasciitis. Patient was treated with surgical debridement, and broad spectrum antibiotics. Patient required IV fluid resuscitation as well. Vibrio vulnificus should be considered when patients have a rapidly progressive soft tissue infection after exposure to salt water related injury.
*3 Vibrio infection
*6 Management of Vibrio Infection
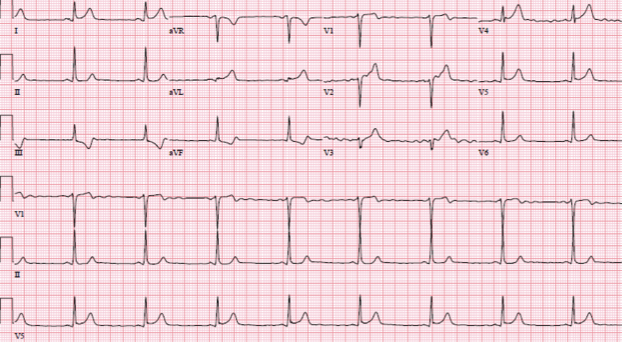
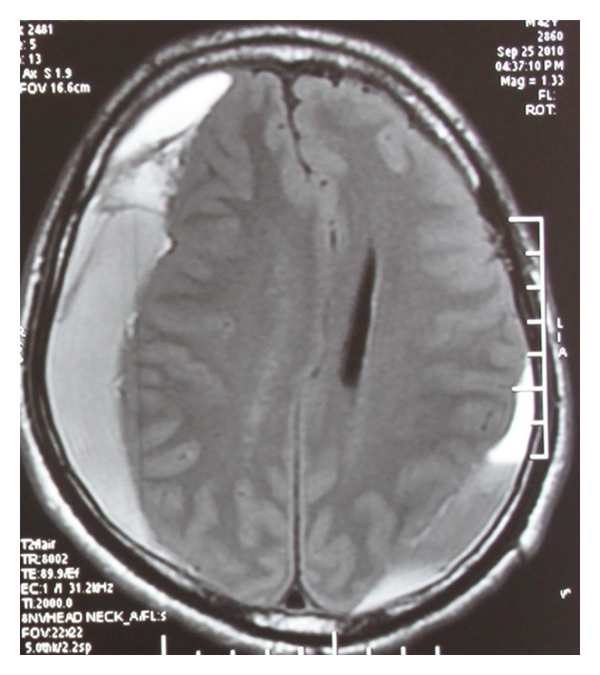
Case 2. 21yo male has a syncopal event. Vitals are basically normal except HR of 101.
*4Patient Had Lown Ganong Levine Syndrome.
*5 LGL EKG
Case 3. 31 yo male with elbow pain following scuba diving. Patient was diagnosed with decompression sickness (bends). Treatment is hyperbaric oxygen.
Decompression Illness (the bends) Laying the patient flat is thought to reduce the chances that an air embolus will go to the brain.
Study Guide Pediatrics
Treat ductal dependent lesions with Prostaglandin E1. The main side effect of PGE1 is apnea. Consider elective intubation for patients receiving PGE1 who need to be transferred.
Most common cyanotic heart defect is tetralogy of fallot. Key pharse is “boot shaped heart.”
*7 Management of Tet Spell. Christine Kulstad also made the point that intranasal fentanyl may be a good choice rather than morphine.
SVT is the most common cardiac arrhythmia in kids. To treat, first attempt vagal maneuvers. Ifvagal maneuvers fail, try Adenosine 0.1mg/kg (can give 0.2mg/kg for second dose). If you give adenosine 2 doses and still have SVT, consult cardiology for either synchronized cardioversion or amiodarone. Of course if the patient is truly unstable go ahead and cardiovert emergently.
For mild dehydration, kids need 50ml/kg of oral rehydration.
For moderate dehydration kids need 100ml/kg of oral rehydration
Faculty recommended apple juice or Gatorade diluted with pedialyte as a rehydration solution.
For moderate to severe dehydration if you give IV fuids, give 20ml/kg bolus and consider a second bolus to give a total of 40ml/kg.
*8TTP vs HUS . TTP has low ADAMTS13 activity. Treat TTP with plasmaphoresis.
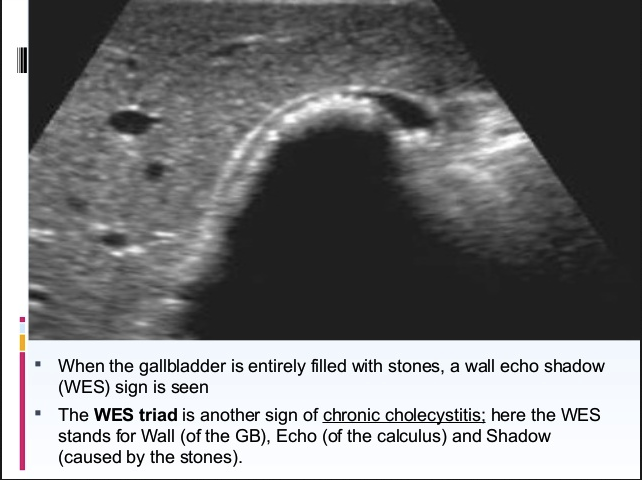
Elise commented on malrotation with midgut volvulus: If a neonate has bilious emesis, you have to get an upper GI. Ultrasound will miss this diagnosis.
*9 Midgut volvulus. Apologies for blurred image but it had the best content.
*10 NEC
*11Pneumatosis intestinalis in NEC(air in the bowel wall)
Treatment of status epilepticus in kids who you don’t have an IV: valium 0.5mg/kg PR, intranasal versed 0.2 mg/kg, IM versed 0.2mg/kg
Elise comment: In seizing kids be sure to check the glucose, sodium, and calcium. Those are the most common metabolic causes.
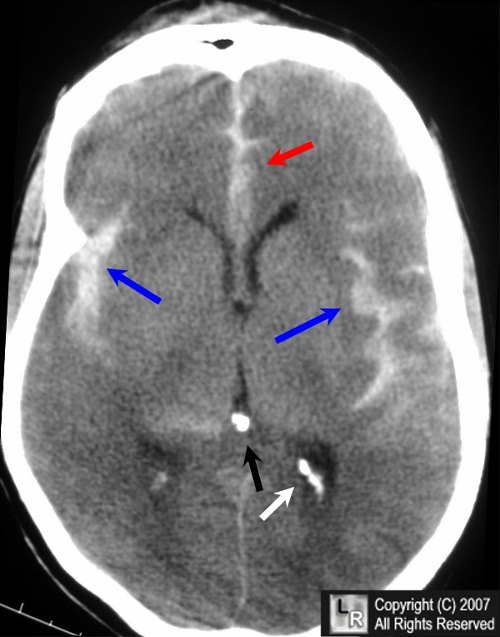
Bernard 5 Slide Follow Up
Patient with AIDS and Pneumocystis Pneumonia
Estimating the CD4 count with the total lymphocyte count is imperfect. 85% sensitivity and 45% specificity for the total lymphocyte count as an estimate of the CD4 count.
LDH is sensitive for PCP pneumonia. Often the level is over 300.
Treatment for PCP is Bactrim first line. Pentamadine second line.
*12 Pneumocystis Pneumonia
Dean 5 Slide F/U
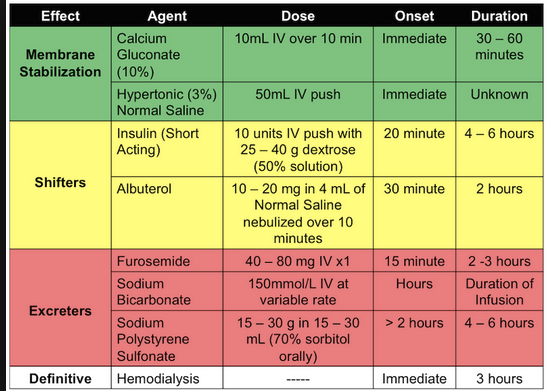
Pediatric patient presents with vomiting and diarrhea. Patient is listless and has dry mucosa. HR=125, BP 78/45. Labs showed metabolic acidosis and elevated lactate. Patient had hyperkalemia and elevated Bun.
Patient initially responded to IV fluids in the ED.
Dr. Dean made the point that you always need to keep up your guard for sepsis and other diagnoses even though the clinical picture looks like dehydration.
Editorial comment: consider QSOFA criteria of tachypnea, altered mental status, and hypotension when considering sepsis.
*QSOFA Criteria. These findings of course need to be considered in the clinical context. Diagnoses like anaphylaxis and hemorrhagic shock can have hypotension with altered mental status and are not sepsis.
Patient was later diagnosed with likely sepsis and treated with IV fluids, IV pressors, IV antibiotics. The patient improved with treatment.
There was discussion among the faculty that this was an unusual and difficult case. But all agreed that a broad DDX is important in ill-appearing pediatric patients.
Dr. Sullivan (visiting professor) Medical-Legal Issues in EM
A report needs to be made to the National Practitioner Data Bank any time there is a settlement, adverse action, or payment made on behalf of a physician. Hospitals must query the data bank when you apply for privileges.
States with the most reports are New York, California, Florida, and Pensylvania.
There are 308,723 reports due to malpractice payments.
Average time from alleged malpractice to settlement is 4.75 years.
Most common allegation of malpractice is diagnostic error.
Residents can and do get named in lawsuits.
The statute of limitations for medical lawsuits is 2 years from the time that the patient or family learned about the issue. This can be extended in pediatric cases.
State Medical Licensure Actions have increased significantly since 1993.
There is a broad range of actions a Medical Licensing Board can take regarding a physicians license.
Judicially tough places for docs: California, New York, Florida, Cook County IL, Pennsylvania
In Cook County, 29% of trials result in plaintiff verdicts. Median verdict $1.1mill. Average Verdict $3 mill. Plaintiffs get half of the award. Plaintiff attorney’s get a 1/3 of the verdict award.
If you ever have to go to trial, don’t tick off the judge. The judge holds the keys to the trial.
There are 4 Aspects of Medical Malpractice: Duty, Breach of duty, Causation, and Damages.
Duty is created by the physician-patient relationship. Phone advice also creates a duty. You may have a duty to other people who may be at risk from a patient (homicidal ideation). If you treat a co-worker who asks for some medical treatment as a curbside. Probably don’t do it. You are creating a duty. The State Medical Regulations require that a chart is created for any medical evaluation/treatment even a curbside.
Breach of Duty examples: The physician failed to uphold the standard of care. If you don’t follow a hospital policy that is a breach of duty.
During depositions be cautious about how you describe your actions. Your statements can be used against you to show that you did not meet the standard of care. Bad outcomes don’t necessarily equate with breach of the standard of care.
Causation means there is a direct causal relationship between the negligent act and the injury. There also has to be a temporal relationship between the negligent act and the injury.
Damages require that there is compensable damages or injury to the plaintiff. Lawyers won’t usually pursue a case for less than $250,000 in damages.
Any battery, or unwanted touching of patient can result in civil and criminal liability. Your malpractice coverage does not cover battery-related liability.
Why do patients sue physicians? Bad feelings toward the physician. Bad outcomes plus bad feelings toward the physician=lawsuit.
Unsatisfactory explanations.
Families don’t want it to happen to anyone else.
Patient’s feelings were ignored.
The doctor made a terrible first impression
The doctor rushed thru the visit too fast
The doctor was rude and insensitive.
80% of malpractice claims are attributed to communication problems
People won’t remember your medical knowledge but they will remember how you made them feel.
Depositions are very important. They are intended to gather further facts, lock the deponent into a certain fact pattern, get an idea of how the deponent will act in front of a jury. You want to present yourself as a caring, responsible doctor. If you can do that, it makes it less likely that you will go to trial.