Conference Notes 3-26-2013
Please consider donating to our EM Foundation to benefit resident education/development. Thanks for your consideration/generosity.
/em-foundation/
Herrmann Trauma in the Pregnant Patient
Bedside U/S will give you a quick assessment of the fetus as far as fetal movement, heart rate and age. Bedside U/S does not give you adequate info regarding abruption. You need to do fetal monitoring to determine the frequency of contractions to guage the probability of abruption. Normal heart rate and no contractions in 4 hours of observation has 100% negative predictive value for abruption.
Pertioneal signs are not as evident in the pregnant patient. Blunt trauma has a higher mortality than penetrating trauma. 0.5 of fetal deaths result from “mild” trauma.
No single imaging study provides a radiation dose high enough to cause harm in a fetus. So image as needed but no more than needed.
Kleihaur Betke test identifies fetal-maternal hemorrhage that exceeds the normal dose of Rhogam (300mcg). If KB test is positive you need to give extra Rhogam.
Left lateral decubitus position when pregnant patient is supine off-loads the inferior vena cava and can treat hypotension.
Peri-mortem C-section: Best results when initiated within 4 minutes of maternal arrest. Goal is to get kid out by 5 minutes of mom arresting. C-section off-loads the IVC and may improve maternal survival, CPR continues during C-section. Make big midline incision (xyphoid to pubis). Hysterotomy through upper uterine segment. Cut through placenta if necessary. Have two teams if possible to divide resuscitative efforts between mom and baby.
Harwood comments: KB test is of less value in 2013 because most RH neg mom’s have gotten a rhogam shot as part of their standard prenatal OB care. Each CT study has to be carefully considered in the pregnant patient. Do the studies that need to be done but no more than that. If doing perimortem C-section make big xyphoid to pubis incision going around umbilicus.
Girzadas comment: If you are looking for a bright line cutoff of which mom’s need fetal monitoring after trauma my suggestion: If a butterfly alights on a patient’s gravid abdomen and the fetus is >20weeks ega, they should have monitoring for 4 hours. Dr. Omi also felt a very low threshold was indicated.
Girzadas Study Guide Arrythmias/Pharmacology
I gave the lecture so I couldn’t do detailed notes, but trust me the lecture was Awesome! :)
Antiarrythmic classification
- 1. Sodium channel blockers
- 1a procainamide, disopyramide, quinidine, tricyclics
- 1b lidocaine, mexilitine, phenytoin
- 1c encanide, flecanide, propafenone
- 2. Beta-blockers
- 3. Potassium efflux blockers- Amiodarone, sotolol, ibutilide
- 4. Ca channel blockers
- Unclassified- Digoxin, Adenosine, Magnesium
There was some discussion on management of arrhythmias/QRS widening/hypotension due to TCA overdose
Harwood comment: TCA caused QRS widening and hypotension can be treated by raising the ph alone. The Na in Sodium Bicarb is not necessarily the key factor. Harwood then discussed the following abstract:
Abstract
Study objectives: We carried out this study to determine the effects of pH alteration on QRS width with administration of tromethamine, a non-sodium-containing buffering agent, in experimental amitriptyline overdose. Design: Prospective, nonblinded trial. Participants: Adult mongrel dogs. Interventions: Pentobarbital-anesthetized dogs were overdosed with amitriptyline 5 mg/kg followed by infusion at 1.0 mg/kg/minute until the QRS width doubled, then decreased to .5 mg/kg/minute until the end of the experiment. At two defined points of toxicity, the dose of tromethamine required to raise the pH to 7.50±.4 was given. pH and QRS width at a speed of 100 mm/second were measured
over a 30-minute period after each tromethamine dose. Data were analyzed with non-linear-regression analysis. Results: At toxicity 1 the mean pH was 7.32, with a QRS width of 11.6 mm. Two minutes after the tromethamine dose the pH rose to 7.51, with narrowing of the QRS width to 8.4 mm. At toxicity 2 the pH was 7.40, with QRS width of 10.6 mm. Two minutes after tromethamine, the pH rose to 7.49 and the QRS width decreased to 9.7 mm. Regression analysis showed a correlation
between pH and QRS width; as pH increased, QRS width decreased (P=.0001). Conclusion: Cardiac toxicity of amitriptyline overdose, as manifested by QRS widening, is reversible by pH changes alone.
Andrea comment: TCA’s are highly protein bound. In overdose situations, changing the ph of the blood will increase protein binding and decrease toxicity. The NA is sodium bicarb can act synergistically on the fast sodium channels.
Mckean/Kerwin Oral Boards
Case 1: Werniecke’s Encephalopathy. Classic triad of Encephalopathy/ataxia/oculomotor dysfunction.is present only 1/3 of the time. Critical Actions: Rule out toxic alcohols, consider disagnosis, give hi dose thiamine 500mg IV Tid.
Case 2: Afib with WPW. Critical Actions: IV procainamide 17mg/kg no faster than 50mg/min. Stop if pt gets hypotensive or QRS widens by 50%. Avoid calcium channel blockers or beta blockers or anything that would block the AV node. That would increase conduction down bypass tract. If patient is unstable with chest pain, hypotension, altered mental status or severe chf then cardiovert.
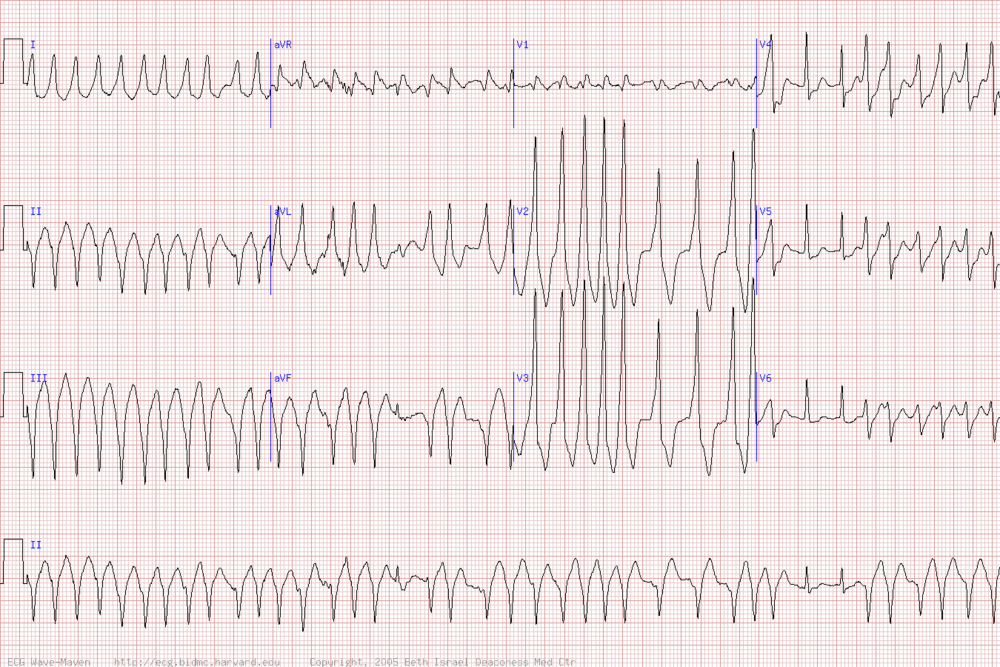
Hemodynamically stable monomorphic VT or pre-excited atrial fibrillation (ACLS, 2010): Loading dose: Infuse 20-50 mg/minute or 100 mg every 5 minutes until arrhythmia controlled, hypotension occurs, QRS complex widens by 50% of its original width, or total of 17 mg/kg is given. Follow with a continuous infusion of 1-4 mg/minute. Note: Not recommended for use in ongoing ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) due to prolonged administration time and uncertain efficacy.
Girzadas comment: consider using only procainamide on the boards for narrow/wide afib or wide complex tachycardia.
Harwood comment: give procainamide 1gram over 30 minutes for your initial managment. This rate will work safely for the majority of patients. If they get better you are done. If they get worse you can shock them or give more procainamde if they have a higher BMI.
Case 3: Toxic Shock syndrome. Fever/rash (sunburn)/desquamation/hypotension/3 or more organ systems. Critical actions: management of shock/abx for staph/remove foreign bodies/surgery for abscesses or localized infections. Kettaneh comment: pt had criteria also for TTP however faculty felt platelets weren’t low enough for TTP. Elise comment: Put the synapse in your brain that shock with a sunburn type rash is toxic shock syndrome. Girzadas comment: think about TSS or Anaphylaxis in the hypotensive pt with vomiting/diarrhea who doesn’t improve with a liter of fluids.

Toxic shock rash from Up to Date

Toxic Shock Rash from Up to Date
Maletich/Gupta Oral Boards
Case 1: Benign Intracranial Hypertension. Critical actions: Do physical exam to find afferent papillary defect and papilledema, pain medication, head ct, LP to check opening pressure. Treatment with acetazolamide is the medical management. Nosek comment: It is unusual to see unilateral eye findings. Rohit agreed. He said findings are usually bilateral but there may be asymmetry of severity of findings from right to left eyes.
Case2: Pyloric stenosis. Critical actions: IV hydration, diagnose pyloric stenosis with U/S, consult surgery, admit patient. Classic metabolic picture is hypochloremic metabolic alkalosis. Hypokalemia takes a couple of weeks to develop.
Case3: CHF/Pneumonia, ARF with hyperkalemia. Critical actions: Treat hyperkalemia, treat CHF and pneumonia, arrange for dialysis.
Purnell Midgut Volvulus
MGV can present with vomiting, hyperglycemia, altered mental status. 2 yo with Initial clinical picture that looked like DKA with a blood sugar of 600 and lethargic mental status. Pt had no ketones in urine. Abdominal exam when pt was resuscitated demonstrated abdominal tenderness/guarding. Xrays showed distended bowel loops. U/S shows free intra-abdominal fluid. Pt ended up with a small bowel resection. He is awaiting small bowel transplant.
Nosek Peripartum Cardiomyopathy (PPCM)
Post-partum patient with SOB/CP/Cough. DDX was mostly between PE and PPCM. Bedside echo showed poor contractility and BNP was quite high. Pt started on carvedilol and low dose lasix, lovenox. PPCM occurs 1 month before or up to 5 months after delivery. 90% occur in the first 2 monts post-partum. Older patients and multparous patients are at greater risk for this problem. Treat with b-blockers/lasix/digoxin. Can’t use ACE-I during pregnancy but ACE-I’s can be useful post-partum. If while pt is ill EF>30%, it is likely pt will regain good EF. Girzadas comment: Lung windows can be a hepful adjunct to cardiac echo. The finding of “headlights in the fog” consistent with extra lung fluid is very reliable. Chastain comment: U/S findings preceed CXR findings. Lovell comment: It is true the CXR findings were not impressive.