Bolton Ethics for the Altered Patient
Deciding whether a patient is competent for decision making is a legal issue. It is decided by a court. ED docs for the most part are not involved in competency decisions.
A patient’s capacity for decision making is a clinical decision. Determining a patient’s capacity for decision making is a common task for ER docs. A mnemonic for to guide the emergency physician is CURVES: The patient needs to be able to Choose and Communicate, Understand, Reason, make Value judgments appropriately, if an Emergency situation exists then you need to act without his consent, If a Surrogate is available, they can consent for the patient.
Molly presented a case of an etoh intoxicated patient with a severe head injury. The patient lacked the ability to choose/communicate/understand and reason. He had no surrogate present. There was an emergency condition present. Appropriate action would be to sedate the patient and get CT of head. There was some disagreement in the audience about whether the physician could also suture the laceration prior to the patient becoming sober and giving consent. Majority felt repairing the laceration while patient was sedated was ethical.
Patients have a right to have untreated chronic psychiatric disorders. However, they can’t refuse treatment for psychiatric disorders and be homicidal or suicidal or not take care of themselves. But if patients have a chronic stable psychiatric illness and they are not suicidal/homicidal/unable to care for themselves they can have the ability to refuse treatment or consent to treatment. Schizophrenics don’t necessarily diminished capacity for decision making. Acutely psychotic patients lack capacity due to lack of understanding and inability to reason effectively.
Suicidal patients are difficult. They may seem to have capacity. Molly presented the case of a depressed 45 yo male who had lost his job, house, and wife. The patient ended up in the ED and told the physician he would go home and shoot himself. Molly said that the patient’s depression impacted on the value part of the CURVES mnemonic. His desire to kill himself is not consistent with his pre-depression value system. From a practical standpoint, failure to prevent suicide is one of the highest payout malpractice categories for emergency physicians. If a patient is at risk for suicide the emergency physician has a duty to prevent suicide.
Next case was a 57 yo female with acute aortic dissection who wants to leave hospital AMA. Pt states she needs to go home to care for her pets. Discussion covered issue that patient doesn’t have capacity based on lack of reasoning ability. Harwood comment: If you can get the patient’s concern solved like getting a neighbor to feed the cats or getting the police to pick up a child at school you frequently can get patients to stay for treatment. Christine comment: I tell the patient that I have the right to keep you here in the ED until you can demonstrate to me that you actually understand and can rationally explain the choice you are making. Elise comment: AMA doesn’t protect you. What protects you is a thoughtful conversation with the patient about their options and risks and carefully documenting that conversation. That conversation and documentation may provide some protection. Kelly comment: if patient leaves against your advice give them good discharge instructions to return at any time and give them the best options for home care. Girzadas comment: Get family members involved as well. They may be able to get through to the patient. Also for risk mitigation involving family members can be critical because they are the ones likely to sue if the patient dies.
Collander M&M
75yo female with chills and leg shaking. Pt is on chemotherapy for stage 4 rectal cancer. She also has polymyalgia rheumatica and is on chronic prednisone. Rectal temp in ED was 39.2. (recent labs were known and pt was not neutropenic so rectal temp was done) BP was 81/50 and heart rate is 115. Lactate was not ordered in the initial order set.
Vitals improved slightly with IV fluid 1 Liter bolus. Pt started on Vanco/Zosyn/Azithro and normal saline at 125ml/hr. Chemo infusion was ongoing in the ED.
BP dropped to 60’s systolic. Pt is tachycardic again. 2nd NS bolus started. Lactate ordered now and comes back 7.7. Pt was transferred to the ICU. She recovered and did well.

If a patient has SIRS and a low MAP give 30ml/kg crystalloid IV . If lactate elevated or pt remains hypotensive after bolus or pt has organ dysfunction then the patient has either severe sepsis or septic shock. At this point, Early goal directed therapy for sepsis is indicated. Elise comment: Scvo2 can be obtained by running a blood gass off of the central line.
Lactate is due to anaerobic metabolism . Lactate is a marker of patient status. If at 6 hours lactate is decreasing, pt’s mortality rate has improved. If lactate has increased, mortality increases. . Blood that sits in lab for a prolonged time can have a falsely elevated lactate. VBG is most accurate lactate
Elise comment: Respect rigors, it is a marker of bacteremia. Harwood: This patient was on chronic steroids for PMR. I would have given stress dose steroids for this patient. Christine/Elise/Harwood comments: If a patient has sepsis fill up the tank with 30ml/kg bolus. Every patient gets this amount of fluid no matter how old, or how frail, or on dialysis, or CHF. The only patients who you don’t give this dose of fluid to are patients who are DNI. If a patient gets volume overloaded you can solve the problem with intubation. DNI patients on the other hand don’t have this therapeutic option available so you will need to be more cautious with them.
Konicki Urologic Emergencies
Urinary retention: Causes include BPH, constipation, prostate cancer, urethral stricture, uti/prostatitis or medications. Use a lidocaine urojet to facilitate catheter placement. Larger Foleys have more stiffness and may be more likely to pass through prostate than smaller foleys. Standard catheter choice for difficult patients is a coudet catheter. Lay the patient completely flat. Pull up the penis to make the urethra as straight as possible. Hold the catheter like a pen. When you hit resistance ask the patient to try to urinate and this sometimes allows the catheter to pass. If you are unsuccessful passing a foley using the above techniques, consult Urology to place foley using the obstructed urethra tray/kit. If you are faced with a significant delay to arrival of urology, you can consider doing an U/S guided suprapbuic tap to drain urine. This is a safe procedure.
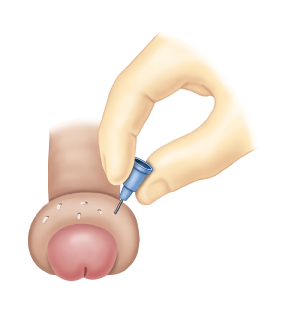
Paraphimosis: Place penile block. Apply compression to penis by hand or with compressive ace wrap for 10 minutes to squeeze out edema. You can also apply sugar, mannitol or dextrose soaked gauze around penis to act as an osmotic agent to reduce foreskin edema. Ice also can aid as a vasoconstrictor on the penis. Once the foreskin edema has been reduced, grab foreskin to reduce over glans. Another approach to reduce foreskin edema is to make multiple small punctures in the foreskin with a 25g needle.
Priapism: Using a non-heparinized 19-gauge butterfly needle, approximately 5 mL of blood should be aspirated to decompress the corpora. Phenylephrine should then be injected into one side of the corpus cavernosum. In adults, phenylephrine should be diluted with normal saline to provide a final concentration of approximately 100 mcg to 500 mcg per mL. One mL intracavernous injections of the freshly diluted phenylephrine solution are administered every three to five minutes until resolution or up until one hour, before deciding whether the treatment will be successful [22]. Lower concentrations and smaller volumes are appropriate for use in children and those with severe cardiovascular disease. It may be necessary to repeat aspiration and phenylephrine injections over several hours to achieve detumescence. (Up to date)

Testicular torsion: Do a bedside U/S with both testicles in the same view so that you can compare them. If they both have similar appearance of blood flow, that is a good thing. If one teste has less flow, you need to be calling Urology emergently. To detorse the teste, you can try “opening the book” . Maletich comment: I reduced a testicle recently. We initially tried open book technique but pain worsened so we rotated in opposite direction and pt’s pain improved and testicle dropped down into normal position.

Bedside renal U/S for renal colic: It helps to lay the patient on the side opposite the pain. Put the probe in the intercostals space of the lower ribs. Elise comment: I would do a CT for a patient who had signs of uti, first time renal colic, suspicion for AAA. Joan comment: U/S or CT imaging is important also to rule out single kidney. Use the color flow Doppler on the suspected kidney, if there are large areas of no flow, that is hydronephrosis
Harwood comments: To deflate a foley balloon that won’t go down with aspirating at the inflation port, you can cut the inflation channel and thread a guidewire down the inflation channel. Paraphimosis can be treated with granulated sugar as an osmotic agent. Priapism can be treated with withdrawing blood from coropora cavernosum and instilling phenylepherine.
Chiefs Sign Out Culture
Discuss any consults with the admitting physician prior to contacting a consultant.
Do not sign out a patient who has vascular access issues or if the techs can’t get labs. Solve these issues before you sign out/go home.
Do the pelvic exam before you sign out the patient.
Just because your attending leaves early or on time, doesn’t mean you leave at that time. You may need to stick around until the end of your shift to get things finished up on your patient.
Don’t sign out a patient with whom you don’t have a plan yet. You need a work up and management algorithm to guide the accepting team. Elise comment: Just be careful that you are avoiding premature closure on a patient. Harwood comment: There are times when you have to dump a patient. If you pick up a patient late in the shift and they need a lot of testing you may need to sign that patient out without a clear cut diagnosis/dispo plan. However, there shouldn’t be more than 1 “dump” per signout.
Update your patients on the plan of management and disposition going forward prior to signing out. You don’t want to leave the receiving team holding the bag with having to discuss the management plan and dispo with the patient.
Anneken Fluids and Electrolytes
Na drops by 1.6 for every 100 mg/dl of glucose over 100.
Hypocalcemia results in long QTc. Hypo k, hypo MG, and hypo CA all cause prolonged QTc. Remember HypO=lOng QTC.
In children with diarrhea restart regular diet as soon as possible. If they are tolerating po there is no need for a BRAT or other form of restricted diet.
Calcium treatment is the fastest modality to treat hyperkalemia. It acts in 3 minutes or less. It stabilizes cardiac membranes but does not decrease K. Insulin/ D50 is the most reliable way to lower K. Albuterol nebs Q 30 min can be effective but 40% of patients won’t respond. HCO3 is only effective if patient is academic. Kayexelate is losing favor and is controversial. It is still being used on a regular basis.
Hypertonic saline for hyponatremia is indicated only for coma, seizures, or focal neuro signs. Also use only in patients with acutely developing hyponatremia such as marathon runners, ecstasy users, or psychogenic polydipsia. If you give it, no more than 100ml at a time and recheck Na every 2 hours. Don’t raise sodium level more than 1 per hour.
Osmolar gap= 2NA + bun/2.8 + glucose/18 + etoh/4.6
Normal anion gap acidosis: adrenal insufficiency mnemonic is USED CAR = Ureteroenterostomy, Small bowel fistula Extra CL Diarrhea Carbonic Anhydrase inhibitoRs
Treatment for hypercalcemia is normal saline followed by calcitonin and biphosphonates. Diuretics no longer recommended.
Acid Base Problems: ABG analysis
Step 1 decide if the ph is academic or alkalemic
Step 2 is the primary process respiratory or metabolic
Step 3 is the an anion gap present?
Step 4 compensation formulas pCo2=1.5(HCO3) +8 pCO2=0.75(HCO3) +20
Step 5 Use other data to help finalize the diagnosis (osmolal gap, lactate level, renal function)
Ted comment: there are only 3 endogenous ways for a patient to develop anion gap acidosis: ketoacidosis, lactatic acidosis, or uremia. All the other causes of metabolic acidosis are exogenous.
We then worked through multiple acid-base problems.
