Hemming/Coghlan Oral Boards
Case1. 65yo female with vague chest discomfort. EKG shows posterior STEMI. However, patient is severely anemic due to GI bleeding. Rectal exam needed to be done to identify the GI bleed. Instead of standard treatment and transfer to Cath Lab, correct management was to avoid heparin/Plavix , give O2 and transfuse.
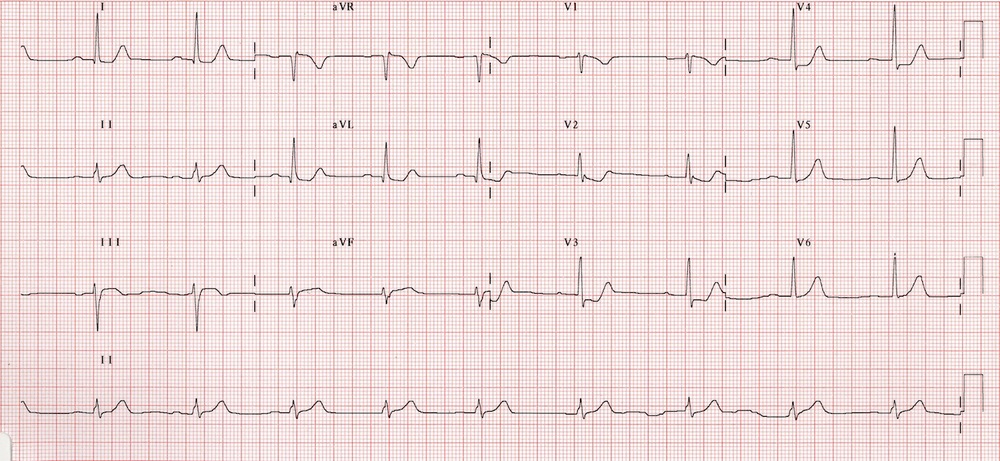
Harwood comment: Posterior STEMI’s in general should go to the cath lab. There is no debate about this as there is with LBBB. This patient, however, was severely anemic so needed PRBC’s not anticoagulation and cardiac cath.
Case 2. 25 yo Female who is 28 weeks pregnant presents with headache. PMH of DVT. Pt is not hypertensive. CT shows cerebral venous thrombosis. Initial treatment is systemic anticoagulation. DDX for pregnant patient with headache: pre-ecclampsia, ccerebral venous thrombosis, idiopathic intracranial hypertension, carotid or vertebral artery dissection, and SAH. Dense triangle sign on a non-contrast CT is a marker of cerebral venous thrombosis.

Dense Triangle Sign

Empty Delta Sign is sign of Venous Thrombosis on contrast CT
Harwood comment: Consider CO toxicity in headache patients. Ask if they have a working CO detector in their home. Reglan (Class B) is preferred over prochlorperazine (Class C) in pregnancy.
Elise comment: Re-frame this case in your mind as a pregnant woman with history of previous dvt and now has a headache. This should point you toward a clotting related disease (cerebral venous thrombosis)
Case 3. 35yo male with eye pain. Flourescein staining shows herpes keratitis. Treatment is viroptic drops.
Girzadas comment: Code word on tests for herpes keratitis is “dendritic pattern on cornea”.
 Herpes Keratitis
Herpes Keratitis
Williamson AICD’s/Pacers
Thanks to Kelly for sharing her images from her slides for the Conference Notes!
Pacemaker leads pass through the subclavian vein into the right atrium and into the right ventricle.
Pacemakers have two primary functions: Sense cardiac activity and provide an electrical stimulus to the myocarium.
NBG Pacemaker Coding: First letter identifies chambers paced. Second letter identifies chambers sensed. Third letter identifies response to sensing. (Triggered, Inhibited, Dual) Example: VVI= ventricular pacemaker, ventricular sensing, Inhibited by ventricular native impulse. DDD=atria/ventricle paced, atria/ventricle sensed, both atria/ventricle can be triggered or inhibited. DDD is the most common type of pacemaker placed currently.
Erik comment: There are new pacemakers that are wireless. Harwood and Erik discussed some of the facets of wireless pacemakers. Basically there are no complications inherent with wires in the body.
Hiccups or muscle twitches in a patient with a pacemaker can be a sign of lead migration.
Most paced ekg’s will have a LBBB appearance due to pacer wire being in the RV. The RV is depolarized first hence the LBBB appearance.
Harwood comment: You frequently have difficulty visualizing pacer spikes on EKG’s in the ED because our ED EKG machines are all set to reduce electrical/movement interference maximally and this will hinder visualizing pacer spikes. The EKG machine’s internal computer will be able to pick up the pacer spikes and the EKG read will say paced EKG even if you can’t see the spikes.
There was a discussion among faculty about where to place a central line in a patient with a pacemaker. The consensus was: don’t place a line in the IJ or SC sites on the ipsilateral side of the pacemaker. Either the wire won’t pass or you risk dislodging a clot or potentially tangling the wires.
Placing a magnet on a pacemaker turns off the sensing function. It puts the pacemaker into an asynchronous mode. It does not turn off the pacemaker. There are not a lot of uses in the ED for this. Probably it would be useful if the pacemaker malfunction is over sensing. The magnet is in the inventory room in a locked cabinet. There is a small risk to changing a pacemaker to asynchronous mode. It could theoretically cause v-fib, but this would be rare.
 Asynchronous pacing causing V-fib
Asynchronous pacing causing V-fib
4 types of Failure: Failure to Capture (spikes not followed by P wave or QRS), Failure to Pace (no spikes) , Failure to Sense (inappropriately placed spikes that are falling within native rhythm), or Pacemaker Caused Tachycardia (Runaway pacer which is pretty rare)
 Failure to Capture
Failure to Capture

Failure to pace
 Failure to Sense
Failure to Sense
Purnell and Herrmann comments: Hyperkalemia can adversely affect pacemaker’s ability to capture or pace.
Pacemakers can develop pocket or lead infection and this can be a very serious infection. 20-30% thrombosis rate associated with pacer but these are most commonly asymptomatic.
Sgarbossa Criteria are helpful in identifying STEMI in a patient with a paced EKG.

AICD Issues: You can get a small troponin leak from an AICD shock. Patients are instructed normally to not go to ER if they are shocked and asymptomatic. Asymptomatic patient with a single shock can go home after discussion with cardiologist. Pt’s who receive multiple shocks or have chest pain need to be evaluated in the ED and most likely admitted. Electrical storm is 3 or more shocks in 24 hours. Electrical storm has a high mortality due to deteriorating malignant arrhythmias.

If you determine that the AICD is giving inappropriate shocks, place the magnet on the AICD for 30 seconds to turn off the AICD. If you do this, put the transcutaneous pads on in case the patient has V-Fib. Taking the magnet off the AICD does not turn the AICD back on. You have to take the magnet off and then replace the magnet on the pacer to 30 seconds to turn the AICD back on.
Asynchronous Pacing causing V-fib
Frazer Trauma Lecture Fire Related Injuries
Case was presented of a patient rescued from a house fire with severe acidosis and markedly elevated CO level.
Smoke inhalation has a 40% mortality. Smoke inhalation is a greater predictor of mortality that BSA burned.
Dry air does not conduct heat well below the vocal cords. So airway burns from dry air are predominantly in the upper airway. Steam inhalation conducts heat 400X more than dry air and can severely burn lungs. Most people with steam inhalation die before getting to the hospital.
If you see evidence of significant airway burn, intubate early to avoid airway obstruction due to worsening edema. Faculty discussion on the significance of singed facial hair: Consensus was that if patient only has singed eyebrows/hair/beard and were not in an enclosed space fire they are not at risk for airway obstruction. The example given was someone lighting the barbeque who has a flash burn is not at risk for severe airway edema. Patients rescued from an enclosed space and/or if they have any other signs such as pharyngeal edema, stridor, or carbonaceous sputum, intubate them early.
CO poisoning: Displaces O2 from hemoglobin, shifts the oxy-hemoglobin dissociation curve to the left , binds myoglobin, and inhibits cytochromes. Symptoms include headache, nausea, syncope, seizure, arrhythmia, death. Identify CO toxicity in the ED with ABG with CO-OX or finger probe device. High normal cut off for the finger probe is 6.6%.. Anything over that get an ABG or VBG. Elise and Christine comment: VBG is a reliable and less painful alternative to ABG for identifying CO poisoning. Hyperbaric treatment is indicated for CO poisoning with a level over 25%, pregnancy, syncope, neuro symptoms, cardiac ischemia, acidosis.

 CO shifts the Oxyhemoglobin Curve to the Left
CO shifts the Oxyhemoglobin Curve to the Left
Hydrogen Cyanide (HCN) Poisoning: byproduct of burned plastics, nylon, cotton, wool, polyurethane. It is a cellular poison that blocks cytochrome function. ABG shows anion gap acidosis and lactic acidosis Treat empirically for patient with smoke inhalation and high lactate or anion gap acidosis. Treatment is hydroxycobalamine 5g IV for adults and dose can be repeated once. Pharmacist comment: This is a drug that is stocked in minimal amounts. You may have to call other hospitals or the poison center if you have multiple patients come in who are all poisoned by HCN from a fire. Second choice is sodium thiosulfate. Andrea comment: HCN is pretty rare in the ED because the vast majority of patients die at the scene.
Elise comment: If you chose to resuscitate a victim of a house/industrial fire and they have significant acidosis you pretty much are obligated to give them empiric hydroxycobalamine.
Carlson
Antidote for acetaminophen toxicity is n-acetylcysteine (NAC). It regenerates glutathione, free radical scavenger, detoxifies NAPQI, and detoxifies parent compound. 150mg/kg IV, then 50mg/kg at 4 hours, an 100mg/kg at 16 hours.
Anthi histamine toxidrome is tachycardia, fever, mental status change, dry mucous membranes, urinary retention. Antidote is physostigmine. Trade name for physostigmine is Antilerium.
Phenazopyridine (Pyridium or Azo) when taken in excess can cause methemoglobinemia. Patients will have cyanosis and pulse ox is usually 85% whether they are on R/A or O2. This is due to the way the pulse ox reads methhemoglobin via light wavelength. Benzocaine (Ora Jel) can also cause methemoglobinemia.
Dextromethorphan is a semisynthetic derivative of morphine. Acts at NMDA receptor and has dissociative effect. It turns a drug screen positive for PCP. Ketamine also turns a drug screen positive for PCP. So if drug screen is positive for PCP, it could be due to PCP, dextromethorphan, or ketamine. Treat the dextromethorphan overdose patient with benzos.
Caffeine binds to the adenosine receptor and can block adenosine’s effects. In the setting of SVT with caffeine overdose, adenosine may fail. For unclear reasons cardioversion has also been reported to fail in the setting of caffeine overdose. Calcium channel blockers or benzos have been reported to be successful in treating SVT in this setting.
Iron poisoining: treat if patient is symptomatic and level is over 350 ug/dl. Treat all patients with levels over 500 ug/dl.
Percentage of iron: Gluconate 12% Sulfate 20% Fumarate33%. If patient ingests >60mg/kg this dose will usually get you a level over 500ug/dl. No need to get TIBC in the setting of Iron overdose because TIBC is unreliable. Treatment is deferoxamine until acidosis clears.
Elise comment: If patient has no gi symptoms in first 6 hours, they will not have a serious ingestion. Example is a child with uncertain ingestion who mom brings in 4-6 hours later and is asymptomatic. No blood testing for iron level needed.
Vitamin A toxicity can adversely affect the brain and the liver.
Goody’s Powder and BC powder for toothache contains ASA and can cause salicylate poisoning. Bengay and Peptobismal and Alka-Seltzer all have ASA in it. Pediatric beptobismal does not have ASA . Blowfish tabs for hangovers, have a large amount of salicylate in them. Look for mixed acid base disorder to diagnose ASA toxicity. Tinnitus is pretty reliably noted by patients with levels over 20mg/dl. Alkalinize urine to get ASA out of CNS.
Burns Case Follow Up
40yo male with acute abdomen and shoulder pain. CT abdomen shows splenic rupture. Pt had no hx of abdominal trauma.
Atraumatic splenic rupture is rare and can be life threatening. 93% of atraumatic splenic rupture cases have a pathologic spleen. Mortality is highest in patients age>40, hx of neoplasm, and splenomegaly.
If patient with splenic rupture and intra-abdominal bleeding is unstable, they go to OR. If stable, they go to IR for splenic artery embolization.
Kehr sign is shoulder pain due to diaphragmatic irritation.
Bonder Case Follow Up
55yo male with altered mental status. Septic picture with fever/tachycardia/hypotension. Patient was being treated for sepsis but no definite source was identified. CPK was ordered and was 70,000. Diagnosis was neuroleptic malignant syndrome due to new antipsychotic (Seroquel). Patient responded well to bromocriptine. Remember to consider non-infectious causes of fever in your differential.
