Updates from previous conference notes:
From Cindy Chan:

*TPA risk/Benefit Analysis
This is final outcome measured at 3 months of 100 patients who received tpa compared to placebo:
- 65% (white figures) did no different
- 32% (light and dark green) did better; 13 of these (dark green) were normal or nearly mml
- 3% (light and dark red) did worse
** 6% (figures with (-) ) had brain bleeding at some point, but at final outcome at 3 months, 3% improved to be no different than non-tpa & 3% did worse
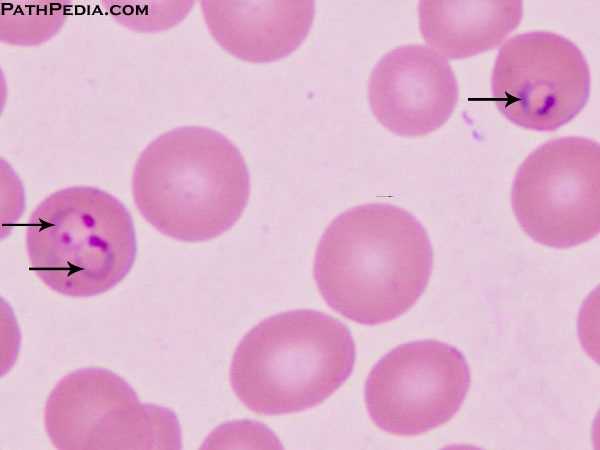
Frazer/C. Kulstad Oral Boards
Case 1. Child presents with recurring fever for 10 days. Child recently traveled to Africa with parents who are missionaries. Pt had an abnormal blood smear DX: Falciparum Malaria Critical Actions: Get blood smear, admit to ICU, treat with anti-malarials (extra points if you knew IV quinidine gluconate plus doxycycline or clindamycin). Initially malaria can present with influenza-like symptoms. Fever occurs at intervals. Anemia and jaundice are common. Disease presents within about 2 weeks of returning back from endemic area. Smear microscopy (thick and thin) is gold standard for diagnosis. Treat mild disease with malarone. If the patient is ill-appearing give IV quinidine gluconate plus doxycycline or clindamycin. Patients need to be managed in ICU due to possible arrhythmias from medications.
Harwood comment: You might want to order a procalcitonin level in this case. It would be elevated in malaria and help you differentiate the case from a viral illness.
*Falciparum malaria on blood smear
Case 2. 28yo female with right shoulder pain after falling while running on a trail. X-ray shows no definite fracture but on Y-view patient has signs of a posterior dislocation. DX: Posterior shoulder dislocation. Critical actions: Get X-rays including Y-view of shoulder. Treat pain/ Use procedural sedation to reduce dislocation. Posterior dislocations are much less common (2%) than anterior dislocations (98%). Classically posterior dislocations occur due to electrocution or electroconvulsive therapy. Traction/counter-traction is the preferred method of reducing a posterior dislocation.

*Posterior shoulder dislocation
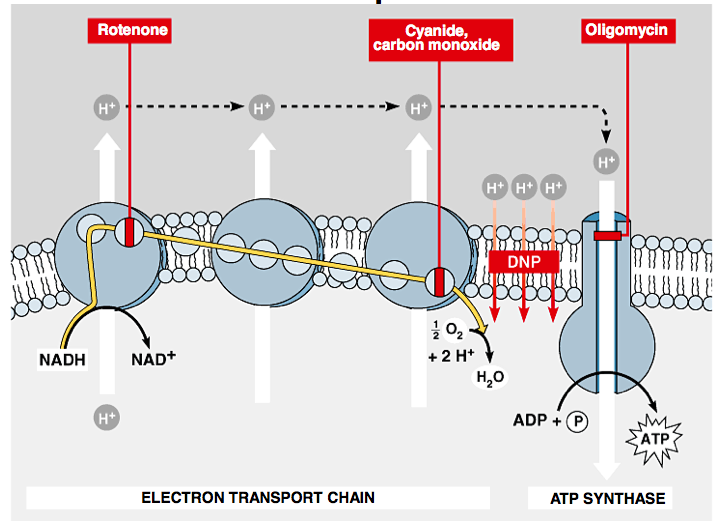
Case 3. 22y female presents after being rescued from a fire in a carpet warehouse. Patient is bradycardic and borderline hypotensive. She is unresponsive. No evidence of any burns. ABG shows severe metabolic acidosis. DX: Cyanide Poisoning Critical Actions: Intubation, get ABG with CO-OX, treat suspected cyanide poisoning with cyanocobalamin. Screen for COHB and MetHB. Cyanide is common from fires involving plastics, rugs, chemical plants, electroplating. Cyanide blocks cellular respiration by blocking the cytochromes. A lactate greater than 10 in a patient rescued from a fire is a strong marker of cyanide toxicity. Also think of cyanide in a severely acidotic patient with a normal SPO2. Co-administration of sodium thiosulfate with cyanocobalamin may have a positive synergistic effect.
*Mechanism of cyanide poisoning
Knight M & M
80 yo male presents with vomiting and diarrhea. O2 sat is low. He was hypotensive and tachycardic. More history elicited that patient had a cough and chest pain. We also learned that the patient just got out of the hospital yesterday. Patient had history of c-diff and gastric outlet obstruction. He recently had a balloon dilatation of gastric outlet.
Patient was made a code 44 to expedite his management.
Airway decision making: We considered intubation to Protect airway, decrease work of breathing. However, patient was oxygenating well and his work of breathing improved with oxygen mask. So initially was not intubated.
IV fluids started. BP was initially fluid responsive. We suspected sepsis and considered pressors. First line pressor is norepinephrine, second line is epinephrine, 3rd line is vasopressin.
Initial EKG did not show STEMI. Initial CXR shows no significant acute change other than possible infiltrate on right. HCAP antibiotics started. Labs showed a high lactate. CBC showed leukocytosis.
At about 2 hours into ED stay, BP drops again to 80/64. Breathing became more labored. With this change, patient was intubated. A left IJ line was placed. Some resistance was noted when line was being placed.
When placing central lines: Always use U/S guidance. Trandelenberg can improve visualization and increase diameter of IJ. Don’t use any force to place the wire.
Post central line CXR shows possible small pneumothorax on left side (the side of IJ placement). To make matters worse. Patient develops an air leak around the ET tube. Patient has to be re-intubated. ABGS show worsening oxygenation. The team then places a mini-chest tube on the left side. Coffee ground fluid drains from the tube. So the team replaces the mini-chest tube with a 34F tube. 1400ml of Coffee ground fluid drains out of the left pleural space. Next CXR shows improvement on left side but patient now has right side pneumothorax. There had been no central line attempt on the right side.
Meanwhile, Pt arrests. ROSC obtained with CPR and epinephrine.
At this point, family decided to withdraw care and patient died in the ED. Diagnosis most likely was boerhaave’s syndrome due to esophageal or gastric tear from previous balloon dilatation. Boerhaave’s syndrome has high mortality up to 72%. Iatrogenic boerhaave’s can have a 19% mortality. Perforations in the lower esophagus have a higher mortality.
Treatment for boerhaave’s syndrome: supportive care, early broad spectrum antibiotics, NG drainage, airway management, chest tube for urgent decompression, and surgical consult.
Harwood comment: You did not cause a pneumothorax. You used U/S guidance to place the central line. The air in the chest was due to the esophageal/gastric perforation.
Elise comment: You can get better information from your consultants if you carefully guide them by specific and well-directed questions.
Girzadas comment: You did not cause a pneumothorax in this patient and based on his initial presentation/lactate/age/co-morbidities you had no chance of saving him.
Burns Safety Lecture
57 yo female presents with cough and sob. Patient was treated with a med neb and felt better. Patient was discharged. After patient was discharged it was learned from a triage note that the patient was sent to the ED for an abnormal EKG. The ED physicians then attempted to find the EKG. The patient indeed had an abnormal EKG. She was called at home and asked to come back. Patient was too tired to come back. She came back the next day but left without being seen due the long wait.
Katie walked us through the system pathway for how EKG’s in our ED are processed. Short version: it is very complicated. There are many steps with no specific person having total responsibility for managing EKG’s. There are many potential ways this could impact patient safety. We then discussed how to improve this system. The most promising suggestion was to give the ED phsycisians access to the EKG computer in the CC hallway.
Carlson Pediatric Toxicology
Causes of Pediatric Toxicology Deaths: #1 fumes/gases, #2 Analgesics, #3 Cold Preparations
Andrea’s pet peaves: Don’t put toxins in drinking containers. Grandparents put their medications in non-child proof containers.
Child resistant means a 5yo can’t open a container in 15 minutes.
When evaluating a suspected pediatric toxicology case find out all the people who live in the house with the child or who watch the child. Any of these adults may be using medications or drugs that the child could get into.
Which exposures should an emergency physician worry about? Calcium channel blockers (diltiazem, verapamil, and amlodipine are the worst), camphor oil (high concentration and has been off the market since the 1980’s), clonidine/visine (imidazolines), TCA’s, Opioids, Lomotil (diphenoxylate and atropine), methylsalicylate (oil of wintergreen, ben gay), sulfonylureas, detergent pods (esophageal burns/perforation), and toxic alcohols. Button batteries are dangerous for kids as well. Button batteries in the esophagus need to be removed within a few hours. It can’t sit in place overnight. Button batteries in the stomach can be watched with serial x-rays. If it has not passed into the bowel by 4 days it needs to be removed. Intranasal batteries or batteries in the ear canal need to be removed immediately.
Also worry a lot about methadone, colchicine, paraquat, amanita mushrooms, and cyanide toxicity.
Don’t worry about: brodifacum (decon rat poison), chlorox bleach, ACE-I’s/ARB’s, diuretics, cholesterol meds, antibiotics, OTC camphor rub/lip balm products (they have low concentrations of camphor) motrin, H2 blockers, Actos, Avandia.
It is always OK to not decontaminate pediatric patients. If you give charcoal to kids be sure it does not have sorbitol. It works best to flavor charcoal with chocolate syrup.
Kernicke-Sklar Malpractice and Discharge Instructions
The most common cause of malpractice is a missed or delayed diagnosis. The second most common cause is an inadequately developed discharge plan. The majority of claims involve a patient who was discharged home from the ED and ended up suffering a complication.
Discharging a patient is in effect a patient handoff. Your discharge instrutions can serve as a good patient care summary that the patient can give the follow up doctor. Discharge instructions are viewed in the legal system as a contract document. Verbal instructions are not good enough. Instructions must be written.
We need a template to reduce our risk related to discharge.
Mnemonic: WTF, DR. DC?
*Anna’s mnemonic
W=what we found/what we did not find. This includes incidental findings. You need to inform the patient that they need to follow up for a lung nodule or other finding on imaging or lab testing. If not, and patient develops cancer or other problem you are liable for that problem.
T=treatment and tests done and still needed. Examples: get your blood pressure re-checked, hold your metformin for 48 hours after CT scan.
F=follow up. Try to be specific as possible. If a patient doesn’t have their own doctor, The Family Medicine Clinic and Adult Medicine Clinic have availability to see patients within a few days.
D=drugs, drug warnings. The physician prescribing the medication is responsible for warning patients about side effects and interactions. Anna puts this info in as a comment on her pre-printed prescriptions.
R=restrictions of activites
D=diagnosis. Just the facts. Don’t make a specific diagnosis without solid evidence. Always include incidental findings in the diagnosis list. Things like pulmonary nodule, elevated blood pressure, colonic wall thickening in the diagnosis list demonstrate that you identified these things and advised the patient to get follow up.
C=come back if…. Be specific as possible with symptoms and signs that would prompt return to ED.
?=final checks. Check the vital signs, ambulation, and for persistent severe pain.

*AMA
Leaving AMA falls under informed consent. Need to do 4 things: 1.Discuss risk/benefits/alternatives. 2.Patient had opportunity to ask questions. 3. Patient demonstrates an understanding of the issues. 4. Patient has capacity to make the decision.
Try to convince the patient to stay. AMA still is considered a discharge.
*Decisional Capacity Assessment
Anna and Elise comment: we always put in our note that we encouraged the patient to stay in the ED and to return to the ED as soon as possible.
Document re-exams. Address abnormal vital signs. Address incidental findings found on imaging and labs.
Be aware of your own biasises and how they affect your judgment.
LIU New Observation Program for Unattached Patients
Call the IM resident phone for any next-up OBS admission to the CDU. Admit to Dr. Nand on the bed request. If a patient has HMO insurance or goes to an advocate clinic they will not go into this service.