BG: ph=7.0, PO2=200, PCO2=30, HCO3=5. FIO2=100% O2 on ven
If you don't see images scroll to the bottom and click on "read in browser"
Jeziorkowski/Girzadas Oral Boards
Case 1. 55yo male presents in coma. The patient is found to have an anion gap metabolic acidosis and an osmolal gap. Urine shows calcium oxalate crystals and EKG has prolonged QT interval. Patient was diagnosed with ethylene glycol toxicity. Patient was intubated for airway protection. Fomepizole was given to block alcohol dehydrogenase. Nephrology was consulted for emergent dialysis. Optimal care included a bicarb drip and thiamine and pyridoxine co-factors given to optimize metabolism of glyoxylic acid.
n Anion Gap = Na-(CL + HCO3) and should be 15 or less
n This Case: 140-(105 + 5)=30
CAT MUDPILES mnemonic for anion gap acidosis
Cyanide, CO, CHF
AKA, Aminoglycosides
Theophylline, Toluene, Tylenol
Methanol
Uremia
DKA
Paraldehyde, propylene glycol
Iron, Isoniazid, Inborn Errors
Lactic acidosis
Ethylene glycol, Ethanol (lactate)
Salicylate, Starvation Ketosis
Case 2. 7 yo male shot in right thigh during a drive-by shooting. Patient was resuscitated with IV fluids 20ml/kg and IV PRBC transfusion of 20ml/kg. Patient did not have hard signs of vascular injury. Patient did have abnormal ABI of right lower extremity. CTA of right thigh showed vascular injury. Patient went to OR.
Hard Signs of Vascular Injury mandate operative repair
Pulsatile bleeding
Pulsatile hematoma
Bruit/thrill
Absent pulse distal to injury
Ischemic signs (pain, pallor, coolness, paralysis)
EAST Guidelines
Hard signs should prompt surgery without angiogram
ABI <0.9 or other soft signs should get CT angiography
CT angiography is the primary diagnostic study
No Hard/soft signs and normal ABI can be discharged
Case 3. 4 yo male fell in pool and was submerged for 1-2 minutes. When rescued, patient coughed and started crying. There was no loss of consciousness and no required resuscitative efforts. On arrival to the ED , the patient had normal mental status, normal vital signs, clear lungs, pulse ox =97% on room air and CXR was normal. Patient was observed in ED for 4-6 hours and remained asymptomatic. Patient was discharged home.
- A patient that was immersed in a liquid and suffered any sort of respiratory event is considered to have suffered a drowning
- Asymptomatic patients with clear lungs, normal pulse ox, and normal CXR can be discharged after 4-6 hours of observation.
- Criteria for Admission(altered mental status, abnormal vitals, P/O<95, respiratory symptoms, abnormal lung sounds, abnormal CXR)
Htet M&M
There are studies to document that morbidity and mortality in teaching hospitals increases during July and August. It is a real phenomenon.
Case: 65 yo male presents with hematuria. He is also hypoxic and hypotensive. Patient is on warfarin for atrial fibrillation.
Labs showed an INR of 7 and a lactate of 5. WBC= 13.6. HGB=8. CXR showed a RLL infiltrate and effusion and a possible small right side apical pneumothorax.
FEIBA and vitamin K was given. Patient was also treated for pneumonia/sepsis with Ceftriaxone and Azithromycin.
Later that day, patient dropped his pressure and became hypoxic. He deteriorated further into a PEA arrest. A chest tube on the right was placed during resuscitation out of concern for possible worsening pneumothorax and pus came out in the tube.
Diagnosis was empyema and warfarin coagulopathy.
Dr. Htet’s Teaching Points:
- Intubate early in course of illness
- Consider CT of Chest to further evaluate the lung findings of pneumonia/effusion.
- Consider a chest tube early if empyema is in the differential diagnosis.
- Pursue the cause of shock aggressively. Elise comment: An ABG can be useful to help determine the cause of shock. The Emergency Physician should set for themselves time limits to get the patient out of shock. If the time limit is not met more aggressive measures need to be started.
- Harwood comment: I agree the ABG is an underused tool for figuring out the cause of sepsis. Rechecking the HGB is important. If the HGB is falling below 8 in a patient with and elevated troponin, transfuse.
- Harwood comment: If you have a sick patient with an infiltrate/pleural effusion and on the same side the patient has a small apical pneumo (air in the hemithorax) you need to consider empyema.
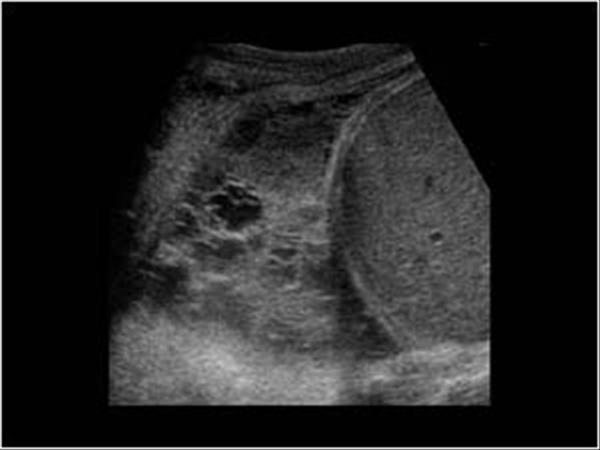
Bedside ultrasound is a good way to identify if patient has an empyema.
*U/S of empyema
Empyema needs to be drained. Think of it as an abscess in the chest, or similar to an obstructed/infected kidney. All these pus collections need emergent drainage.
4 reasons to intubate
- Protect airway
- Failure to oxygenate
- Failure to ventilate
- Ease the work of breathing
Bottom line if you see a patient with pneumonia and pleural effusion do a CT or bedside ultrasound to differentiate empyema from para-pneumonic effusion. If you identify empyema, thoracentesis or chest tube to drain the empyema is indicated.
Burt Acid/Base 4 Step Method of Analyzing an ABG
Step 1. Identify abnormal values on the ABG
Step 2. Calculate the anion gap
Na - (Bicarb + chloride)= Anion Gap
Step 3. Apply the Rule of 15
Bicarb +15 should = the PCO2 and Last two digits of the pH. This step will identify a “hidden respiratory” process. As an example if the PCO2 is higher than expected by the rule, there is a respiratory acidosis in addition to the primary metabolic acidosis. If the PCO2 is lower than predicted by the rule, there is a respiratory alkalosis.
ABG: ph=7.1, PO2=200, PCO2=30, HCO3=10. FIO2=100% O2 on vent
Bicarb +15 = 25. Based on the rule of 15 the pH should be 7.25 and the PCO2 should be 25. However the measured pH is 7.1 and the PCO2 is 30. Because the PCO2 is higher than predicted by the rule there has to be a respiratory acidosis in addition to the metabolic acidosis.
Step 4. Calculate the Delta Gap
Subtract the delta gap (AG – 15) from the normal expected bicarb (24) to identify the predicted bicarb.
If actual measured bicarb is higher than predicted then there is a hidden metabolic alkalosis. If the actual measured bicarb is lower than predicted then there is a hidden metabolic acidosis.
Example: Anion Gap =25, Hco3 = 15. 25-15=10. 24-10=14. The actual measured bicarb (15) is pretty close to the predicted bicarb (14) so there is no “hidden” metabolic process.
Example 2: Anion Gap= 30, HCO3= 20 30 -15 = 15 . 24 -15 =9 The predicted bicarb (9) is less than the measured bicarb 30 indicating a “hidden” metabolic alkalosis in addition to the metabolic acidosis.
Elise comment: The delta Gap calculations (Step 4) are difficult and rarely will make a clinical difference in the ED. You probably can get by with the first 3 steps alone.
VBG’s and ABG’s have reasonably similar values for ph, pco2, and bicarb. The PO2 is the value that is significantly different between an ABG and VBG.

*ABG vs VBG
Parker ACS

*STEMI vs NSTEMI

*Posterior EKG

* Antero- Lateral STEMI

*Inferior STEMI

*RV Infarct (III with more ST elevation than II. Also ST elevation in V1)
Inferior STEMI’s tend to have bradycardia and blocks. They can have papillary muscle rupture. Overall inferior STEMI’s tend to do well.
Anterior STEMI’s tend to develop CHF, shock, wall rupture, and malignant arrhythmias. Anterior STEMI’s have higher mortality than inferior STEMI’s
Right ventricular MI’s are very volume dependent and can develop hypotension. Be very cautious with IV NTG. Give fluid boluses to support pressure.
Treatment of STEMI’s : ASA, Nitroglycerin, Heparin are the basics.

*Sgarbossa Criteria for diagnosing AMI with LBBB or Paced EKG
Myers Administrative Lecture
EM Doctors and nurses should meet and update the patient together prior to discharge or admission.
Be careful when ordering cervical/vaginal diagnostic studies. Frequently the wrong swabs are sent. Be careful to label your specimens. On the Label, note the time you actually obtained the sample. Samples need to be sent to lab within one hour of being obtained. If the test was ordered initially but then later you decided not to gather samples, cancel the order. When obtaining GC/Chlamydia samples use the blue swab only. The current CDC recommendations state you can swab anywhere in the vaginal vault to obtain GC/Clamydia samples. You don’t have to swab the cervix. Give the patient the time frame of 7-10 days for GC/Chlamydia results.
If you are swabbing an extra-genital site for GC/Clamydia you have to use an E-swab for GC culture and UTM (universal transport media/influenza medium) for chlamydia culture. You don’t use the GC/Chlamydia swabs we use for vaginal/urethral testing on extra-genital sites.
Medication reconciliation is critical to patient safety. A good resource for patients’ medications is in Firstnet. Under Orders, click on “external medication references.” When the window opens up, you may have to click on refresh multiple times to get the list. You can also click on “medication list” under Orders in Firstnet. Use other resources as well: patient, family, nursing home records, prior records, and primary physician.
Elise and Kelly comment: It is the physician’s responsibility to identify the medications the patient is on that could be possibly causing the acute condition. It’s not the physician’s responsibility to put the list into the computer, but in the end we are responsible for identifying critical meds like warfarin or rivaroxaban.