E. Kulstad Research Update
ACMC EM is #1 in the world in enrolling patients with intra-cerebral hemeorrhage and hypertension into the ATACH 2 Trial! Please continue to enroll these patients in the study.
The Macy Catheter can be used to give almost any medication rectally. You can give up to about 500ml of water or pedialyte per hour rectally. This may be a therapeutic bridge option in the person who has a difficult IV access.
C. Kulstad Study Guide Cardiology
There is no mortality benefit to routinely taking non-STEMI, ACS patients to the cath lab. Thus, the patient with chest pain and bumped troponins and a non-STEMI EKG gets equal benefit from medical management as they would from going to the cath lab.
The absolute mortality risk reduction of ASA in ACS is 4%. This data is derived from the 1988 ISIS study that showed ASA brought mortality down from 13% to 9%. The absolute mortality reduction from heparin and LMWH in non-STEMI ACS is 0%. The data for heparin and LMWH in STEMI is not known. There is no Cochrane review on this topic. We don’t really know the mortality benefit, if any, for heparin in STEMI.
POISE-2 study showed that you should hold ASA prior to abdominal surgery. There is no increase in mortality if you hold ASA prior to abdominal surgery in patients with prior MI. If you give ASA prior to surgery there is an increase in bleeding. Elise comment: Most surgeons should not have a problem limiting surgical bleeding due to a patient’s ASA use.
*Electrical alternans is a poorly sensitive and reasonably specific finding of pericardial effusion.
Stress echo is a moderately sensitive (80%) and specific (80%) test for coronary stenosis. It however is not a good test to identify risk for major adverse coronary events (MACE)
A murmur at the right 2nd intercostal space is consistent with aortic stenosis. These patients can present with chest pain, dyspnea and exertional syncope. It is a murmur that is easy to miss. The prevalence of aortic stenosis in the elderly is 3% (pretty high prevalence). There is now a new option of transcatheter aortic valve implantation that allows for valve replacement therapy without thoracotomy.
*Indications for temporary and permanent pacemaker
Hi dose NTG has shown mortality benefit in CHF. We probably under dose IV NTG. One strategy to get a higher dose of NTG into a patient is to use sublingual spray. Each spray gives 400micro grams per spray. You can give a spray every few minutes in the hypertensive, pulmonary edema patient.
Tobacco cessation is the single most profound risk reduction strategy in patients with CAD.
Pericarditis pain is worse lying down. Patients can also have pain with swallowing.
Burns/C. Kulstad Oral boards
Case 1. 24 yo male presents with agitation and hyper-adrenergic toxidrome. Patient had to be restrained by EMS personel and was fighting against restraints. His troponin and AST are elevated. His CK is markedly elevated. Urine tox screen is positive for cocaine. Patient management of cocaine overdose required relatively high dose IV benzo’s for agitation and hyperadrenergic vital signs. Treatment for cocaine toxicity is benzodiazepines as your first/second/third line. Patient also required IV fluids for rhabdomyolysis. A bicarb drip for cocaine-induced rhabdomyolysis is controversial. Cooling measures were also indicated to manage hyperthermia. Avoid beta-blockers in cocaine toxicity. You can get unopposed alpha effects.
Case 2. 28 yo female with left shoulder pain.
*Image
Diagnosis was AC joint separation. Treatment is sling, pain control, and non-emergent orthopedic referral. You have a two-week time frame to surgically repair an AC separation. AC joint separation is the most common shoulder injury in athletes. High-grade separations require surgical repair.
Xray findings of AC separation: The acromion is not level with the lateral clavicle.
*AC separation Xray
Case 3. 20 month old female brought in for crying.
*Monitor strip
Exam shows enlarged liver. Patient has cool extremities.
Diagnosis was SVT. Treatment was IV adenosine 0.1mg/kg initial dose. The rhythm slowed temporarily but then returned to SVT. Second adenosine dose was 0.2mg/kg, which also did not convert the patient. Child appeared more clammy/shocky so the next move was synchronized electrical cardioversion. Patient was given intransal fentanyl prior to cardioversion. Initial shock was 0.5j/kg. Patient converted with first attempt at cardioversion. If first attempt fails you can go to 1j/kg.
Remke Pediatric SVT
Case 1. 7 day old with a heart rate of 300. BP 75/47. Afebrile. Patient had been feeding well. Lungs were clear. Color was good. Rythm Strip showed SVT. Child was treated by peds cardiology in the ED with propranolol and rate was controlled.
*3 Types of SVT
To diagnose SVT in pediatric patients, the heart rate should be great than 220 in an infant and >180 in a child. There should be no P waves on EKG. The rhythm should be very regular with no variability. Sinus rhythm has more variability than SVT. Notching of the T wave suggests sinus rhythm with the P wave buried in the T wave.
*Sinus Tach vs. SVT
*Pediatric SVT Management Algorithm
Vagal maneuvers include: ICE to the face, Valsalva maneuver, and rectal stimulation with a thermometer.
For known WPW use procainamide instead of adenosine. Elise comment: For orthodromic narrow complex SVT it is ok to use adenosine even if it turns out to be WPW. It is the AHA recommendation.
Avoid verapamil in infants and children. It is contraindicated in patients under 1 year of age because it can result in V-Fib and hypotension. It can be used as a second or third line therapy for SVT in teenagers.
After cardioversion, admit infants and discharge older kids/teenagers after a 2-4 hour period of observation. If you identify WPW discuss with cardiology about admission for ablation.
Ede Low Risk Chest Pain
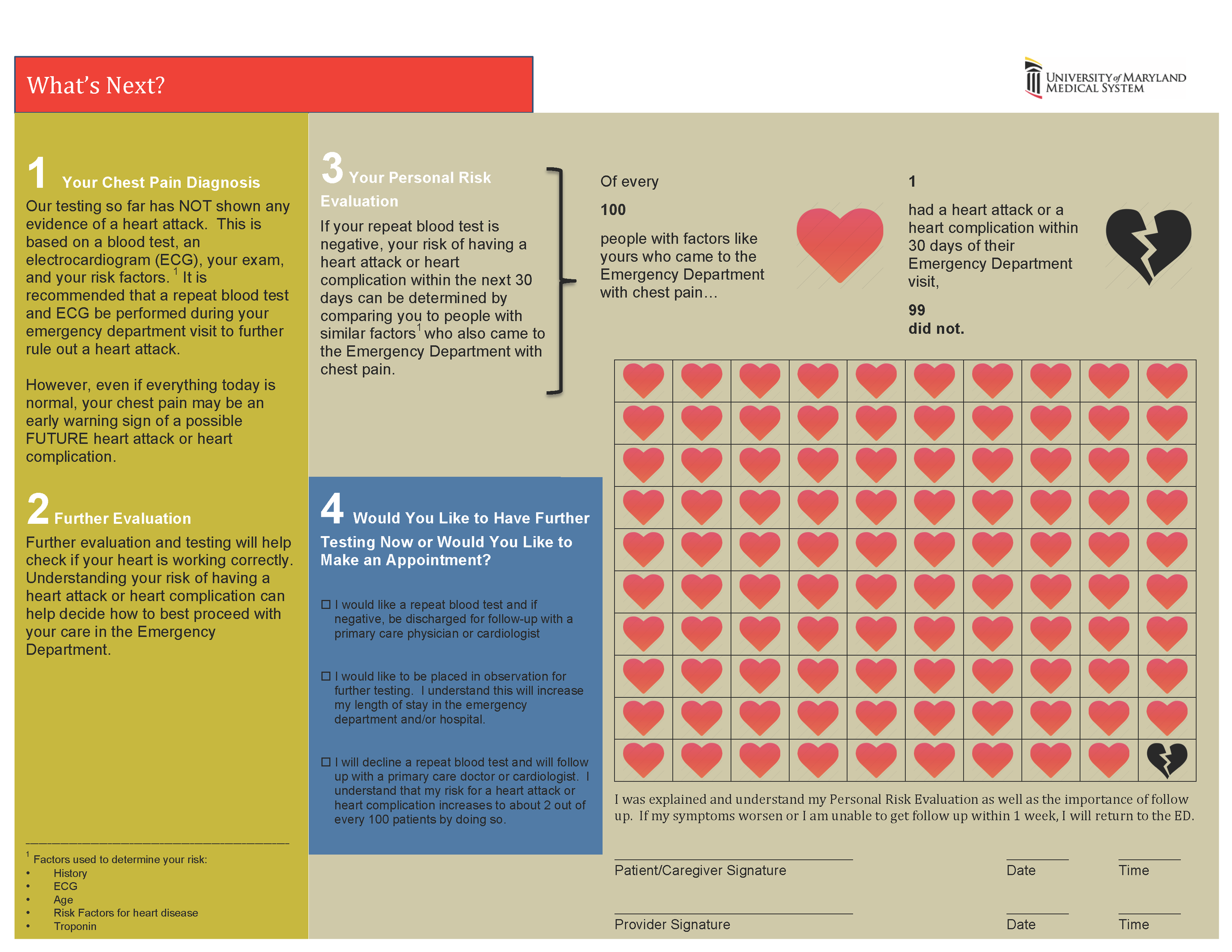
Chest pain patients are considered low risk if the probability of major adverse cardiac events is 1-2%.
Patient’s response to GI cocktail or NSAID or NTG is not reliable for ruling in/out ACS.
Women may have more atypical symptoms.
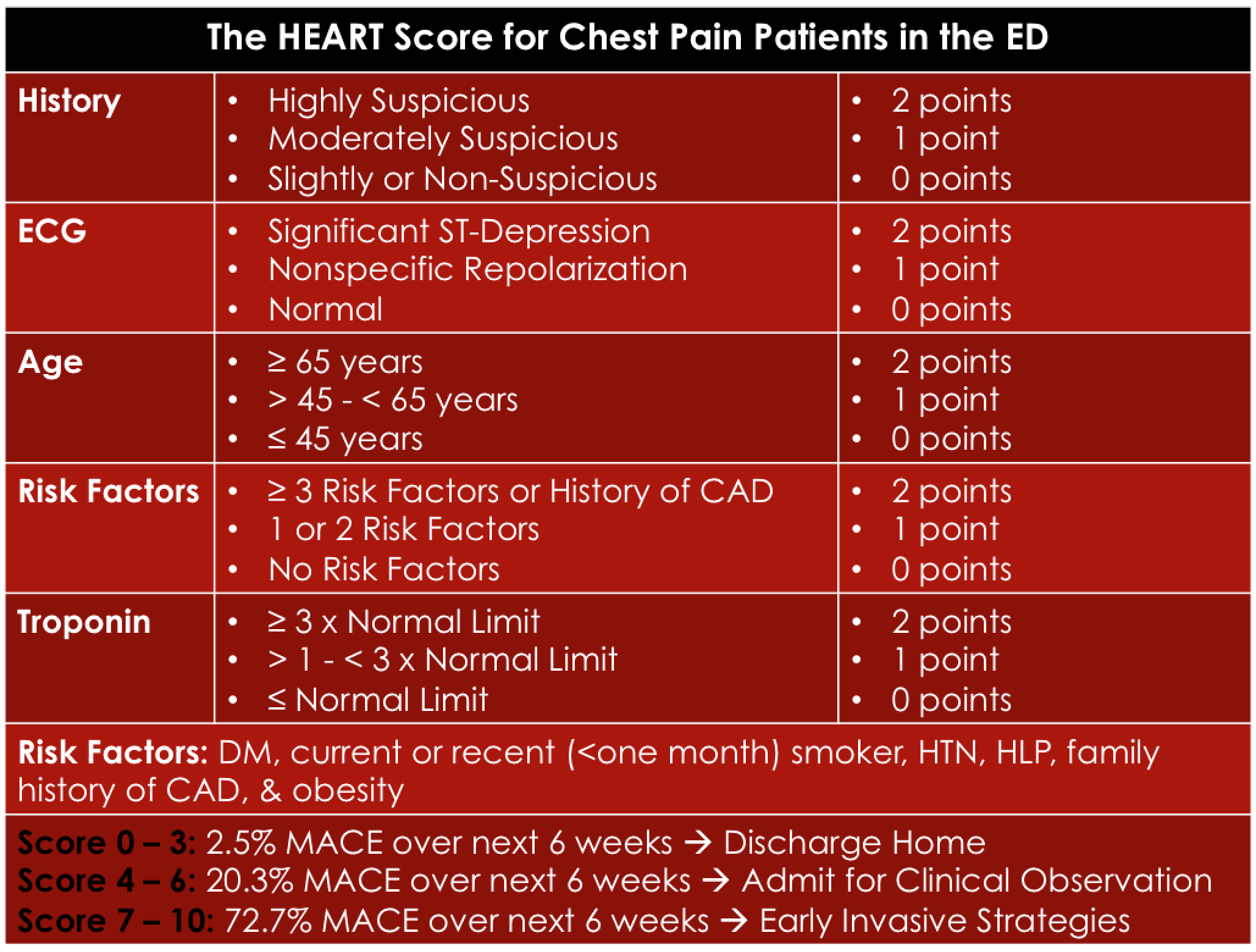
*HEART Score Patients who are low risk by HEART score and have 2 negative troponins 3 hours apart have a less than 1% risk of MACE (major adverse cardiac events) in 6 weeks.
*Heart Score Decision Making
Hart Tachyarrhythmias
*Tachycardia Algorithm. I would only add that procainamide can also be used and is probably preferred for wide complex irregular tachyarrythmias (WPW).
If you have IJ central line access, you can use a lower dose of adenosine because of a faster transit time to the heart. Braden Parker noted that 3mg of adenosine worked quite well in a patient with SVT that he treated through an IJ line.
Adenosine causes a sense of doom or chest pain in patients. You should give some sedation prior to administering adenosine.
*WPW Syndrome
Avoid AV nodal blocking agents (betablockers, calcium channel blockers) in antidromic (wide complex) tachycardias. Blocking the AV node in antidromic tachycardia can result in death.
Aflutter usually has a rate right around 150.
*Atrial Fibrillation and Atrial Flutter
Calcium Channel Blockers have been shown to be superior to beta-blockers for Afib.
*Junctional Tachycardia can be hard to diagnosis. Consider digoxin toxicity when you see Junctional Tachycardia.
*Diagnosing V-Tach
*Girzadas note: Another Approach to Diagnosing V-Tach on ecgpedia.org. I have always struggled with differentiating VT and SVT with Aberrancy. This seems like a simple way to do it. In lead II if the initial upstroke or downstroke of the QRS takes more than a box it is likely VT. A caution, It is not validated yet.
First line treatment for Stable Ventricular Tachycardia is Procainamide. Second line is Amiodarone.
*Torsades Treat with Magnesium or Overdrive Pacing
Parker PodCast Pearls for Codes
Traumatic Arrest is usually due to one of a few things: exsanguination, pericardial tamponade, or tension pneumothorax. Based on that, is there any reason to do CPR for traumatic arrest? CPR can also hinder other activities/procedures being performed on a trauma patient. CPR can increase the risk of blood exposure to the resuscitationist.
Mnemonic for PEA in the Trauma patient: HOTT= Hypovolemia, Oxygenation, Tamponade and Tension Pneumothorax.
C Kulstad and Girzadas comments: We are uncomfortable dropping CPR completely from trauma resuscitation. We think there is medical-legal risk to that. Possibly a more middle of the road approach would be to prioritize life saving procedures. If CPR is hindering other life saving procedures such as gaining IV access, relieving tamponade, or relieving tension pneumothorax stop CPR for as short a time as possible and perform the procedure and re-start CPR as soon as possible.
PEA Management: Use ultrasound to identify causes. If the QRS in PEA is wide think metabolic causes like hyperkalemia, TCA overdose, infarction. If the QRS is narrow think obstructive causes such as tamponade, tension pneumo, or PE.
Jamieson Parasites
A parasite lives at the expense of the host.
The CDC Lists 5 Parasitic Infections we should know.
Chaga’s disease: Caused by protozoan Trypanosomi Cruzi. Acutely, patients have fever and malaise. They can also acutely have eyelid swelling, myopericarditis, and meningitis. Chronically patients can have CHF or megaesophogus. You need to get the treatment drugs from the CDC.
*Eyelid edema from acute Chaga’s Disease
Cystercercosis: You get the worm from eating infected pork. Neurocystercercosis can result in seizures. When the infection is in the muscle if feels like bumps. Treat with albendazole, anti-seizure meds, steroids, and surgery.
*Nueorcystercercosis
Toxocariasis: Caused by ingestion of cat or dog feces. Acutely the patient will get a hepatitis or pneumonitis. The pneumonitis can look like asthma. Kids can also get unilateral visual impairment from fundal involvement.
Toxoplasmosis: Caused by ingesting cat feces. Infection can be spread vertically from mom to infant. Congenital toxoplasmosis can cause spontaneous abortion, fetal death, and fetal neuro deficits. Immunocompetent adult patients can have a mono-like syndrome. Immunocompromised adult patients can get encephalitis.
Trichomoniasis: Most common non-viral STD. Can be asymptomatic for months. Women have vaginal symptoms. 75% of men are asymptomatic. Can result in pregnant women having premature rupture of membranes and preterm delivery.