Reminder Emergency Medicine Foundation Golf Outing Tuesday afternoon/evening, October 8th.
Gupta Study Guide Trauma
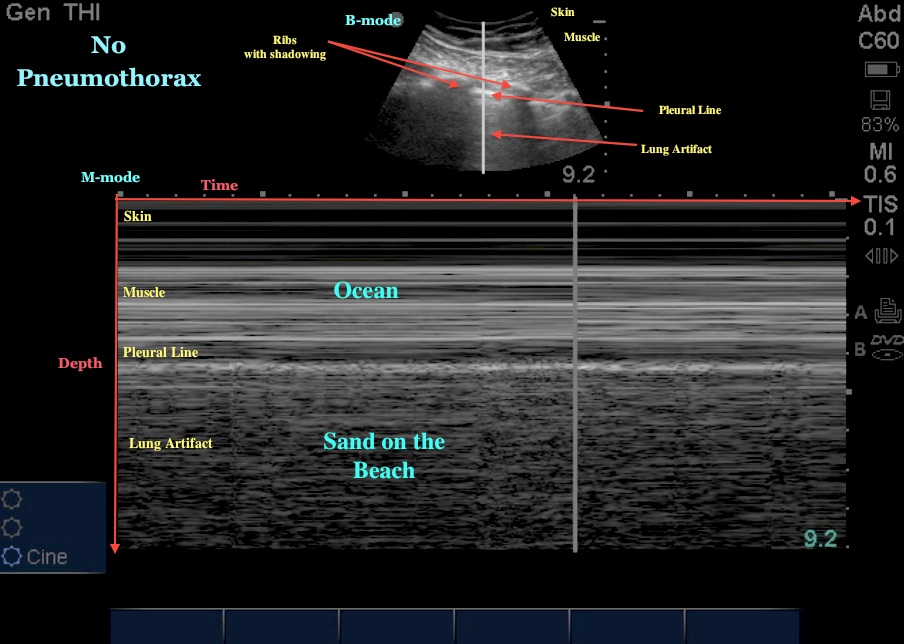
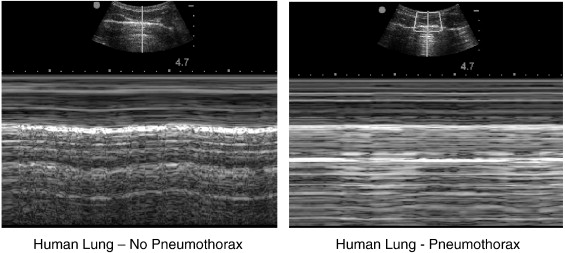
If you suspect tension pneumothorax, do immediate needle thoracostomy. Do not wait for CXR or a clinical response to IV fluids.
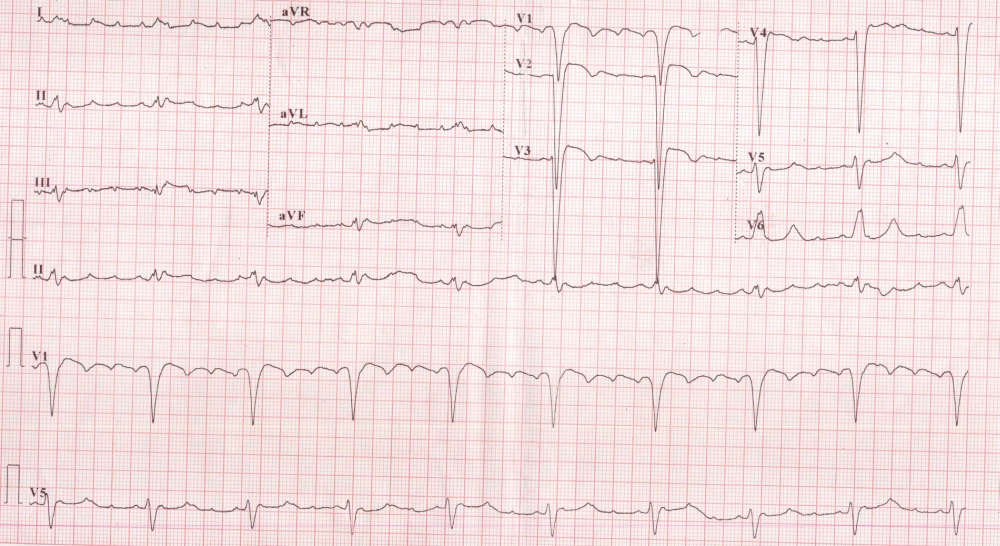
If you are seeing this CXR you are late in needling the chest:

CT is more sensitive/specific than ultrasound for diagnosing solid organ injury. It is more sensitive than ultrasound for picking up small amounts of intraperitoneal blood. CT is not great for picking up hollow viscous injuries. Harwood comment: Use serial exams to diagnose hollow viscous injuries if you are suspicious and CT is non-diagnostic.
Kelly Williamson comment: In adults with blunt flank trauma who don’t have gross hematuria and who are not hypotensive, you don’t need to work up the patient for renal injury. You don’t need to send the urine to the lab. You can visually inspect the urine to check for gross hematuria. If the urine is not grossly bloody, you don’t need to work patient up for renal injury.
In contrast to adults, microscopic hematuria in pediatric patients who suffered blunt trauma still requires further evaluation. Harwood comment: You won’t find a lot of treatable injuries using microscopic hematuria as your only criteria to do a IV contrast CT. Gupta comment: For the boards, microscopic hematuria in adults requires no further urinary tract evaluation. Microscopic hematuria in kids, requires a CT abdomen/pelvis with iv contrast. Elise comment: The injury you would be looking for is at the junction between the kidney and the ureter. This area is very mobile in kids and is prone to injury. Harwood/Elise/Erik/Christine comment: They wouldn’t CT a kid for just a few RBC’s in their urine. The kid would need in addition some history or sign of serious trauma to proceed with CT. There was then a discussion about the recent publication of the PECARN decision instrument to decide on work up of the abdomen in kids with blunt trauma.
Elise comments: Strengths-as always with PECARN, really big study, well done, reliable results. Weakness- they don't incorporate US in their workup (during EMRAP interview with an author he stated that some centers weren't using US routinely). Doesn't specifically discuss microscopic hematuria, but simple 7 point instrument to help decrease CT use in these kids. Decision instrument missed 2 kidney injuries: one kid had gross hematuria, the other had distracting injury (rib fracture) and microscopic hematuria (10 RBC per hpf).
Harwood comments: This is a great rule. It has a 99.9% (-) predictive value & doesn't use micro urine or LFT's (in old rules). It did missed 7/203 injuries (requiring treatment). However, of the 7 misses, 2 kids were 2 y/o's. 1 did indeed have gross hematuria & was treated without an operation (did get a blood transfusion). 5 were 16-17 y/o's. All would have gotten ED CT's based on presentation. This includes a 17 y/o MVA had rib injury, blood in the belly (& 10 RBC's in urine). This pt got got embolization (spleen? most likely).
Intraperitoneal bladder rupture usually results from a compressive force to abdomen causing rupture of dome of the bladder. Gross hematuria is present 98% of the time.

Extraperitoneal bladder rupture is caused usually by sharp boney edges of pelvic fracture.

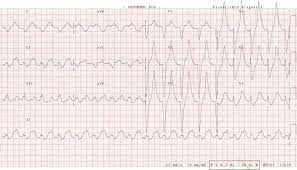
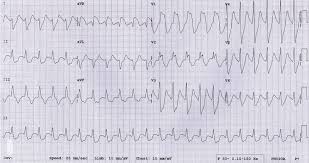
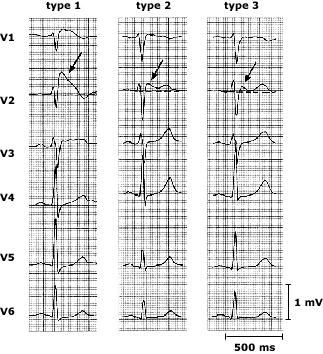
Large myocardial contusions can result in cardiogenic shock. Harwood and Girzadas comment: There is no good diagnostic test for myocardial contusion and there is no accepted treatment for myocardial contusion so there is no point expending resources looking for this. If the patient is in shock you gotta think hemorrhage, hemorrhage, hemorrhage. But if hemorrhage is ruled out and the pt is hypotensive or has an arrhythmia it could possibly be from myocardial contusion but still is more likely to be due to hemorrhage.
The spleen is the most common organ injured in blunt trauma . Blunt trauma; organs most frequently injured in decreasing order: Spleen>liver>kidney>small bowel . Penetrating trauma; organs most frequently injured in decreasing order: Small intestine>liver>colon.
Harwood comment: In elderly patients with multiple rib fractures (3-4 broken ribs) , they have a surprisingly high mortality. Admit them for observation. Christine comment: Mortality in the elderly increases by 19% for every rib broken above 2.
Left sided diaphragmatic hernias are three times more likely than right side. The liver is thought to protect the right diaphragm. Diaphragm injuries can be subtle initially and pt may become symptomatic years later.
Treat patients with pelvic fractures and hypotension with pelvic binding, prbc/ffp transfusion, and angiography with embolization.
Jakubovich Pediatric Trauma M&M
Pediatric GSW victim(5yo) transferred from outside hospital to ACMC. Intubation was attempted at initial hospital but was either unsuccessful or tube became dislodged. Upon arrival at ACMC, pt could not be intubated using laryngoscopy. Resident and attending were also unable to intubate with glidescope. Patient, however, was able to be bag-valve-mask ventilated. ED/Surg team proceeded to perform cricothyrotomy on pt. PRBC transfusion started.
Pt went to OR and had multiple intra-abdominal injuries repaired. In the OR, the cricothyrotomy developed an air leak and was removed. Peds annesthesia was able to intubate the patient.
Patient was discharged home. He suffered from PTSD.
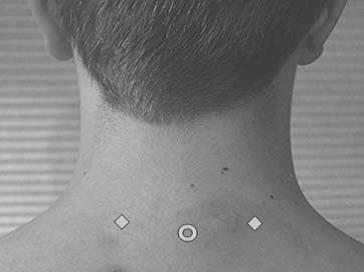
Airway issues: In infants with prominent occiput, you can put a towel under the shoulders to line up the airway. In kids age 5 or older, it is recommended to put a towel under the head to line up the airway. Harwood comment: Place a towel under the shoulders first, if that doesn’t work to line up the airway, move the towel to behind the head and look again.
Pediatric bougie will fit through a 4 ET tube. Adult bougie will fit through a 5.5 ET tube.
Since we were able to bag-valve-mask this patient, did we need to cric this patient? Elise comment: A pediatric LMA may have been a reasonable option in this situation. Our pediatric difficult airway box should have a pediatric sized LMA. Erik comment: Maybe a retrograde intubation over a wire passed through the cric would be a nice technique. Kelly comment: Don’t beat yourself up over doing the cric, you need an airway and getting the airway anyway you can is OK. Christine/Elise comment: If you can bag the patient successfully, you usually have time to consult pediatric anesthesia emergently. There was some consensus among attendings present that an LMA would have been the optimal bridge device until pediatric anesthesia could be consulted.
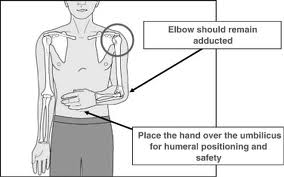
Should we have done an open cric or a needle cric? Age recommendations go down to 5yo for open cric. However at age 5 and below it will be more difficult due to anatomic size. In this case Trauma Surgery had no difficulty passing a shiley through the cricothyroid membrane. Harwood: It is best to use a commercial Melker percutaneous seldinger technique cricothyrotomy kit. Other jerry-rigged needle cricothyrotomy techniques and jerry-rigged jet insuflation are prone to failure. Elise: I agree the Melker kit is the best option. But again, if you can ventilate a patient it is better to continue bagging or place an LMA and get help from anesthesia. Christine comment: Your respiratory therapists will have no experience with needle crics. Erik comment: It may be helpful to remember that in many places around the world, they do entire surgical procedures without intubation and just bag-valve-mask the patient.
Elise follow up comment: We currently stock size 3 LMA in the PED. This is sized for patients weighing 30 - 50 kg, and would work for average sized kids age 8 to small adult.
Getting blood: You can make an MR# for a DOE name prior to arrival of the patient to order blood from Blood Bank.
Kmetuk Cardiac Trauma
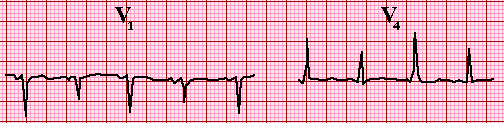
Case 1. Penetrating left chest trauma. CXR discussed by Harwood shows hemothorax despite left chest tube, heart is enlarged and is very suspicious in a young patient for hemopericardium. FAST exam identified hemopericardium. Pt went to OR for repair of RV. Pt did well.
Cardiac Box

RV is the most commonly injured cardiac structure due to penetrating trauma. Penetrating injury to the chest can definitely injure abdominal organs as well. Left ventricle is more likely to self seal than right ventricle. Stab to the heart is 17X more likely to survive than GSW to the heart.
Salzman comment: Patients with stab wounds to the heart are the one’s who can survive an ED thoracotomy. If you do an ED thoracotomy, push the ET tube down the right mainstem bronchus to deflate the left lung and improve your visualization of the heart.
Salzman comment: If you have pressors infusing in a young trauma patient it means they need blood Dammit! Young trauma patients should never get pressors (except possibly neurogenic shock) they need blood.
Salzman comment: You can close wound in the RV with foley catheter, stitches, or staples, or just having someone put a finger in the hole.
Salzman comment: In a 20something patient with penetrating chest trauma, and FAST shows some pericardial fluid, that is blood. Also in a patient who is arrested or peri-arrested don’t hesitate, just get started on the thoracotomy. ( As an aside, when breaking bad news to families, in a similar fashion get to the fact that their loved one is dead with little preamble. ) There is no role for needle pericardiocentesis in penetrating cardiac injury. The blood in the pericardial sac is usually clotted and can’t be aspirated with a needle.
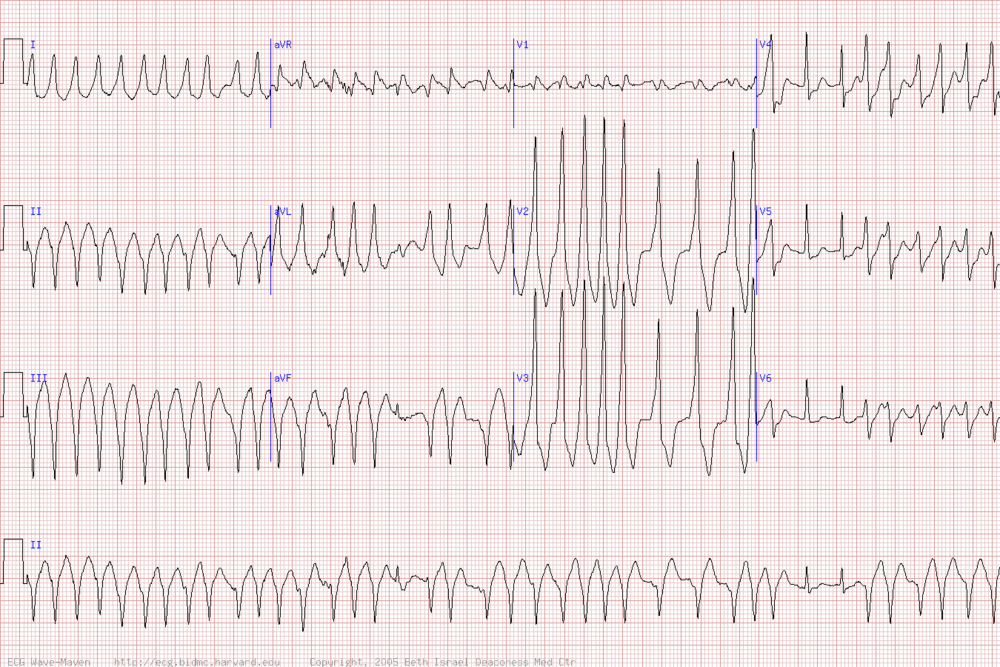
Case 2. 51yo male victim of motorcycle vs. truck collision. Blunt chest trauma. Intubated, hypotensive. CXR shows wide mediastinum. CT chest shows aortic injury. PT was started on esmolol but BP dropped and esmolol was stopped. Pt’s aorta was repaired in the OR with a graft. Pt walked out of hospital 20 days later.
90% of patients with aortic injury will die at the scene. 50% of the survivors die in the next 24 hours.
High risk historical factors for aortic injury: rapid deceleration injury, t strikemvc, fall more than 3 stories.
Febbo question: Do you need to CT scan an asymptomatic patient who has one of the above mechanisms? Salzman comment: Yes, he has seen pt’s who have intimal injuries or pseudoanuerysms that have been relatively assymptomatic.
Walchuk Mandibular Dislocation
Anterior dislocation is the more common dislocation and is reducible in the ED. Posterior dislocations are rare and need specialty consultation and likely OR reduction/surgery.
Pt’s with anterior dislocations can’t close their mouths. There will be a preauricular depression in the skin. Check cranial nerves 5 and 7. Unilateral dislocations will have jaw deviation to the side opposite the dislocation.
Posterior dislocations can result in external auditory canal injury.
Intra TMJ lidocaine can give significant pain relief and even allow reduction.
You can try to elicit a gag response. The gag response blocks contraction of the masseter and can result in reduction of the dislocation.
Dan Gromis method of masseter massage was presented on video. Basically, an assistant massages the masseters on both sides while the operator applies inferior and posterior pressure on the mandible while at the same time tilting the chin upward. The video demonstrated very easy and non-painful reductions.

After reduction, pt should be on a soft diet for a couple of days.
Harwood comment: Main thing is to apply some downward traction on the mandible and get the chin elevated relative to the angle of the mandible and then move the mandible posteriorly.

Lam Fever in infants 0-90 days
Fever/age cutoffs to initiate work up in kids: 0-90 days=38C 3mo-36mo=39C
10% of kids 0-90 days with 38C or higher temp will have serious bacterial illness.
Clear cut national consensus to do sepsis workup and admit/give IV antibiotics in kids 0-28 days. Give Amp and Cefotaxime. Sam said he has the experience of regularly giving ceftriaxone in kids 0-28 days with no complications during his fellowship.
Well appearing infants 29-90 days old with Temp 38 or higher is the difficult group to make decisions on.
Rochester criteria: WBC 5-15K, UA with less than 10wbc/hpf, less than 5wbc in the stool. No LP criteria. Also kids can’t have any significant pmh or clinical exam findings of serious infection. These low risk criteria miss 15-45% of serious bacterial illness..
Boston criteria: WBC under 20k, CSF with less than 10wbc, UA with less than 10 WBC or neg urine dip. All kids got 50mg/kg ceftriaxone IM. All had re-check and second dose of ceftriaxone in 24 hours. These criteria missed 6% of serious bacterial illnesses.
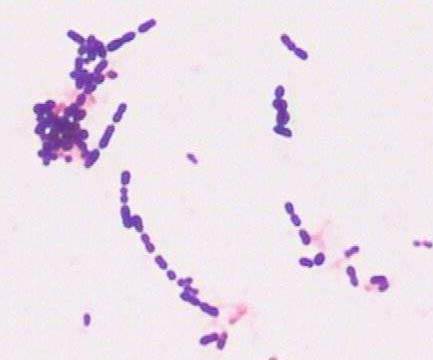
Philadelphia criteria: Non-toxic, WBC <15K, low bands, urine with <10wbc /hpf and no bacteria on gram stain, CSF<8wbc/hpf, CXR with no infiltrate, Stool with not a lot of WBC’s. High risk kids were admitted with antibiotics. Low risk kids did not receive antibiotics and were sent home. This strategy missed the least amount of serious bacterial illnesses.
In this age group there is a 10% chance of viral meningitis.
If you are going to treat a febrile child in this age group with ceftriaxone, you need to do a LP prior to giving ceftriaxone. There is national consensus on this management point as well.
OM does not make a child in this age group low risk. They still need an LP.
Bloody taps require admission and antibiotics because the results are uninterpretable.
Sam uses the Philadelphia criteria in kids less than 8 weeks. He does a full septic workup on them. If results fit low risk criteria, he sends them home. Scott Altman and Sam both said they will give kids antibiotics (ceftriaxone) prior to sending them home.
There was some practice variability voiced in the group. Some faculty will do full septic workup, give antibiotics, and admit for observation in all these febrile kids 0-8 weeks.
Occult bacteremia in kids 3 months to 36 months in the era of pneumo and HIB vaccinations is basically dead. The incidence of contaminated blood cultures is approximately 10X the incidence of positive blood culture. So getting blood cultures in these patients leads to many more false positives than true positives. In Immunized kids 3-36 months with high fever, instead of getting blood cultures, look for uti. A kid with 2-3 doses of vaccine can probably be considered immunized.
In kids in this age group, if you get a CBC for whatever reason and the WBC is over 20K get UA/UCX and get a CXR. Kids with a WBC >20 are at higher risk for both.
Kids who have a clear cut diagnosis of a viral illness(positive rsv, chicken pox, croup, bronchiolitis,etc), meningitis is very unlikely.
Thanks for reading! Stay safe out there. Double glove and be cautious/take your time with procedures to avoid Sharps Injuries.