erratum from last week: Dr. Walchuk gave Study Guide and I did not credit him with his excellent presentation. Thanks Steve!
I will take next week off due to vacation. I will resume the Conference Notes on 8-20
Purnell/Carlson Oral Boards
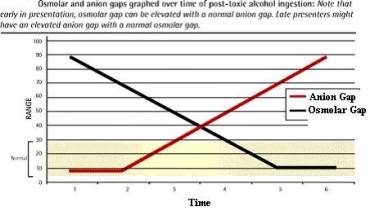
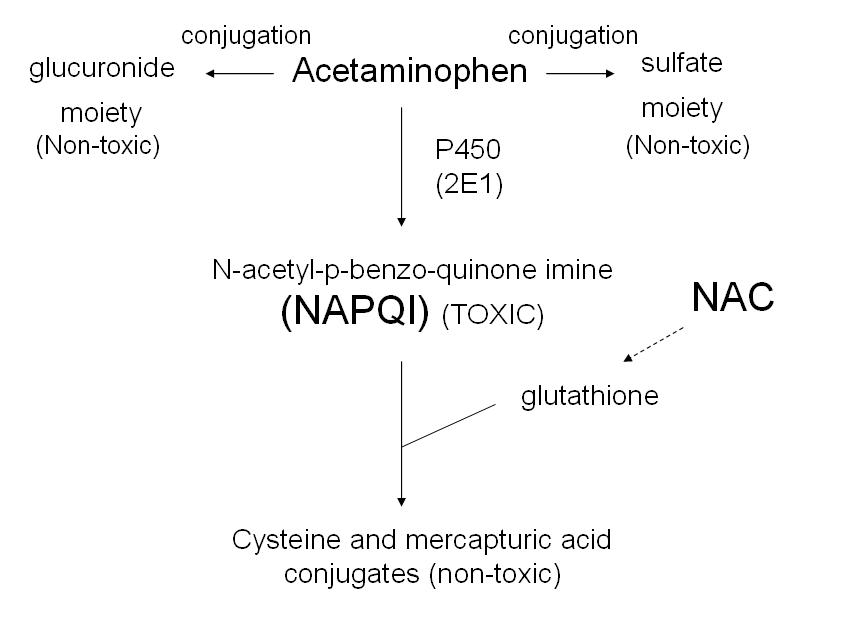
Case 1. 46yo female with possible suicide attempt. Patient is altered with abnormal vital signs of tachycardia and decreased respiratory rate. Pupils were constricted. Pt responded initially to narcan but became sedated again. The patient’s husband brought in the patient’s medications which included a long acting hydrocodone preparation (ZohydroER). Critical actions: Identify opioid toxidrome, give naloxone, exclude co-ingestions such as ASA and APAP, start naloxone drip to manage long-acting opioid, admit to ICU. Optimal care: In any patient who has CNS depression consider getting a serum osmolarity to evaluate for toxic alcohols. Methadone, fentanyl, tramadol, and buprenorphine do not show up on toxicology screens. Zohydro is a controversial new extended release hydrocodone formulation. The concern is that it has much abuse potential and that overdoses will be particularly dangerous. There is no APAP or ASA in Zohydro.
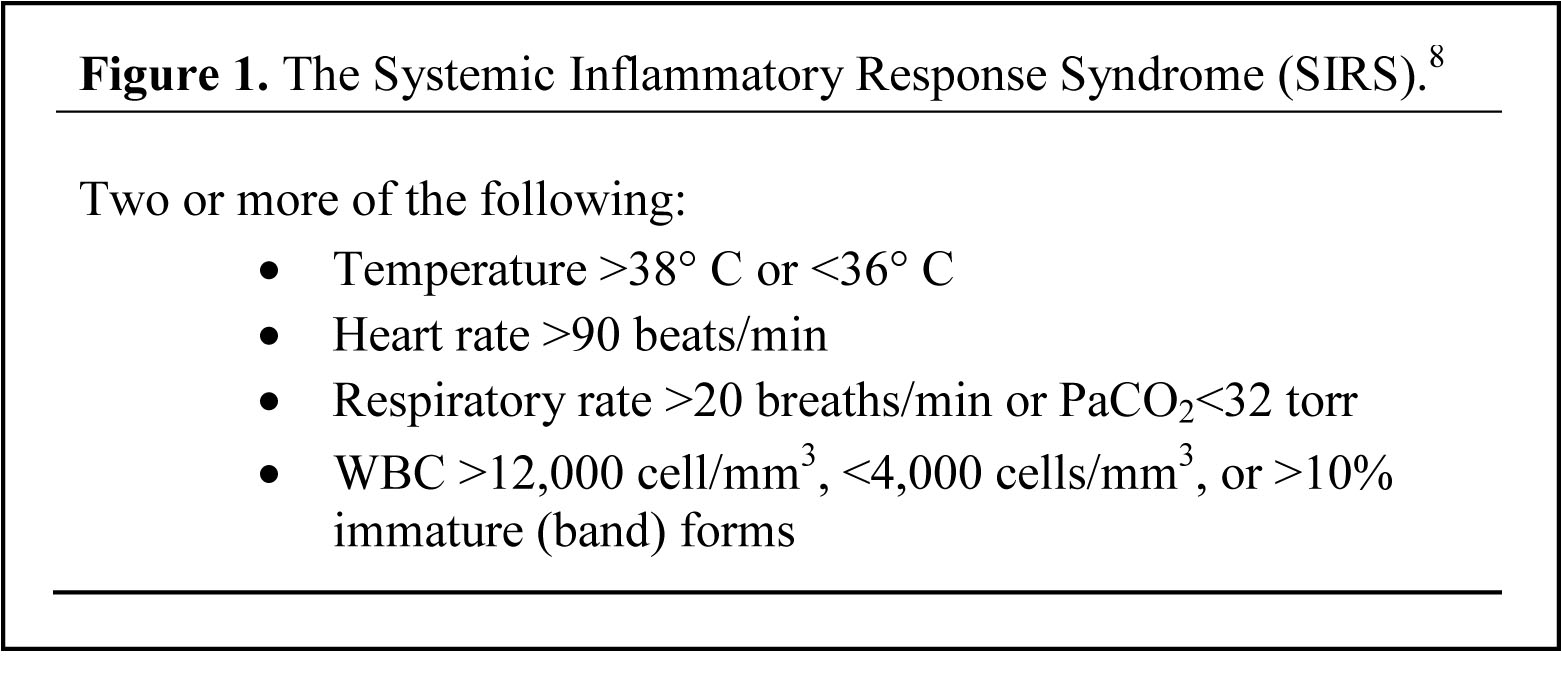
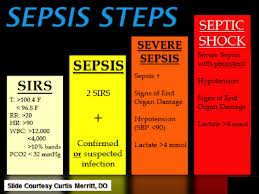
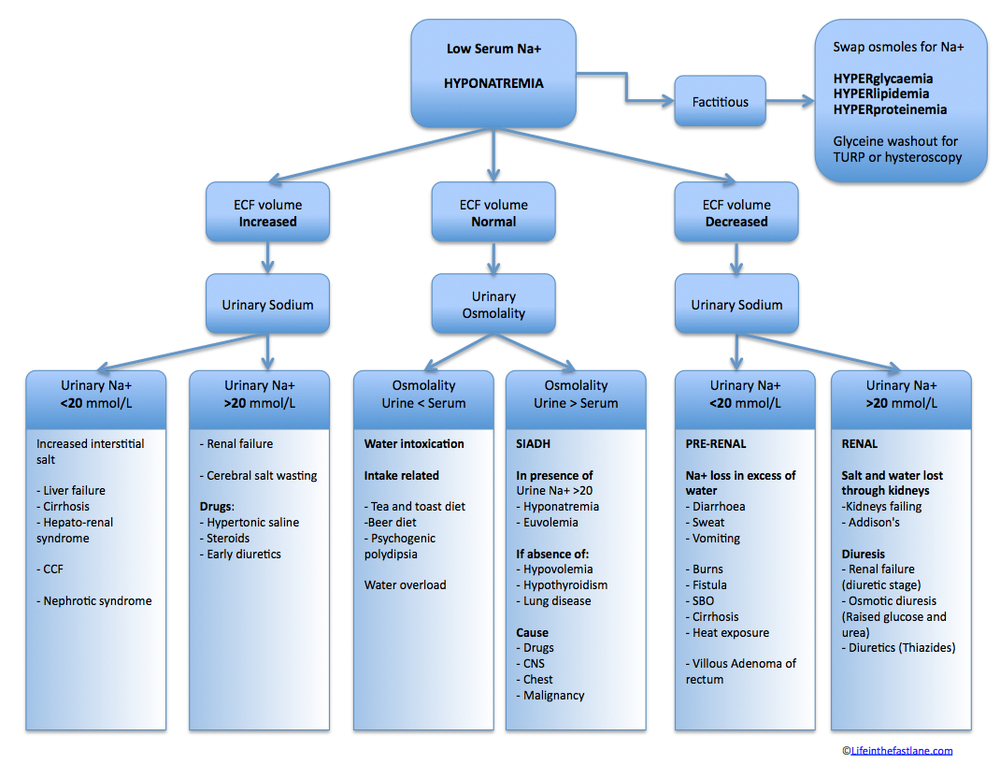
Case 2. 38 yo female with fever, cough, and lethargy for 3 days. On day of presentation, patient has abdominal pain and vomiting. Patient fainted in the waiting room. BP=80/66 P=146 R=28 T=103.5 Patient is on Humira, methotrexate and prednisone for rheumatoid arthritis. CXR showed pneumonia. Labs showed hyperkalemia/hyponatremia suggesting adrenal insufficiency. Critical actions: Get history of steroid dependence and immunosuppression, give IV fluids for hypotension, give steroid replacement (solu-cortef/hydrocortisone is preferred) , treat hypoglycemia, and treat pneumonia.
Elise comment: Would you also investigate other opportunistic infections in this setting? Andrea yes but this can be done as an inpatient. The ED doc needs at a minimum to give CAP antibiotics.
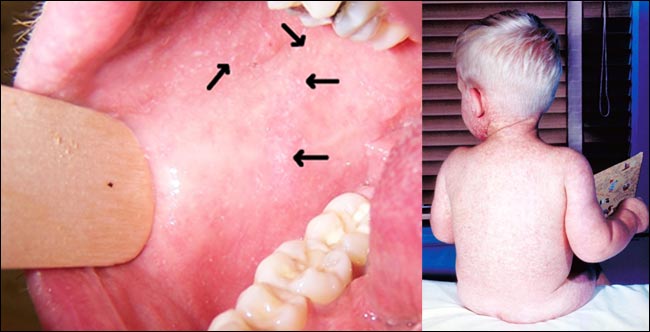
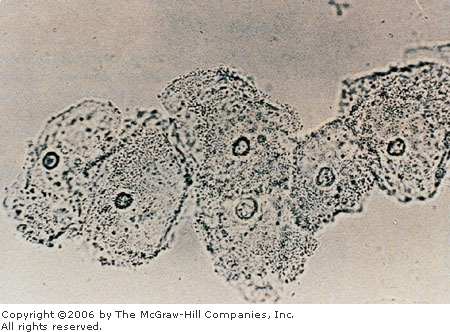
Case 3. 2yo male with fever, cough, rash for 2 days. Patient has just returned from trip to Phillipines with his mom. Child is not immunized due to mom’s mistrust of immunizations. ED diagnosis was measles based on rash and Koplik’s spots. Critical actions: Obtain history that patient was not vaccinated, diagnose measles presumptively, isolate patient for 4 days before and 4 days after onset of rash, send confirmatory testing, arrange treatment for at-risk contacts. In the first 6 months of 2014 there have been 593 cases of measles in the US. There have been 2 cases in March 2014 in Macomb, IL. Incubation period is 7-21 days. 3 C’s of measles=cough, coryza (runny nose/stuffy nose/sneezing), conjunctivitis. Rash starts on face and spreads down over the body over 4 days. Koplik’s spots are pathognomonic but they last only 2 days before or 2 days after the onset of the rash. Treatment is supportive. Ribavirin can be considered in more ill or immunocompromised patients. Vitamin A supplementation is also advised. You will also have to give vaccine or immune globulin for exposed contacts.
*Measles Rash and Koplick’s Spots
Navarrete Trauma Lecture Hand Injuries
Management of finger tip avulsions with no boney involvement: Apply a non-adherent dressing. Soak in warm soapy water for 10min daily followed by tap water irrigation and redress. Repeat this process for 10 days. Have the patient return for a wound check in 2 days. Complete healing can take up to 8 weeks. Re-attaching the amputated portion is rarely successful.
If the finger tip avulsion involves exposed bone, consult hand surgery. Fakhori strongly recommends never ronguring the bone back in the ED. Steve Salzman comment: When you go to your next job and don’t have the resources of a Trauma center. You have to discuss these cases with the consultant and if you don’t have a Hand surgeon available, you have to transfer the patient. Elise comment: If you are working in a smaller ED and patient presents with exposed bone you need to discuss with a consultant or transfer.
Phalanx fractures: Distal phalanx fractures usually don’t require surgical management. Proximal and middle phalanx fractures require precise alignment/fixation and need referral.
Bad hand injuries: Don’t FREAK OUT. Stop the bleeding, control pain, wrap in xeroform and kerlix, give IV antibiotic coverage (Ancef), update tetanus status, get imaging, and consult hand surgery.
Calling the Hand Surgeon: Tell them the patient’s hand dominance, careful NV exam, extent of injury, tendon/muscle/bone exposure, and fractures. Texting a picture is probably the most informative. You have to get consent from the patient allowing you to text a picture of their injury to the hand surgeon. Document their consent in the chart. Elise comment: after texting the picture, delete the picture from your phone to protect patient confidentiality.
There was a discussion about using low dose ketamine 0.25 mg /kg in addition to opiates to treat intractable pain. Ketamine lowers opioid needs and is hemodynamically neutral. Dr. Navarrete used keatmine in one of her trauma patients with a severe hand injury and had good success.
Storing amputated digit for re-attachment: wrap digit in saline gauze, place it in a plastic bag, put the bag on ice, and keep the amputated digit with the patient. Christine comment: The ED has coolers available to keep the amputated part with the patient so it is not lost. Salzman comment: Most amputations of digits and limbs are not viable for re-attachment.
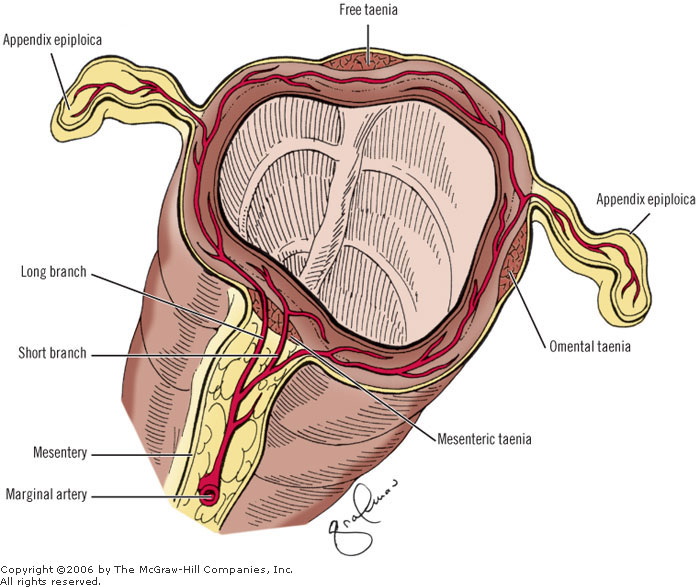
Compartment syndrome in the hand is possible. There are 10 compartments in the hand. Red flags indicating compartment syndrome are bad pain, weakness, tense tissue.

*Hand Compartments
Main message for hand injuries: Treat pain, give antibiotics, wrap the hand, and CONSULT HAND SURGERY!
Campanella The Dizzy Patient
Peripheral vertigo is usually not continuous but rather episodic. Episodes usually last less than 1 minute
Dizziness that last minutes to hours: consider meniere’s, TIA, migraine, psychiatric, otic syphilis
Mnemonic for Vertigo DDX: VITAMIN C=Vascular, Infectious, Trauma, Autoimmune, Metabolic/Medications, Idiopathic, Neoplastic, Congenital like Arnold chiari malformation.
Differentiating Vertigo from other causes of dizziness: With peripheral vertigo, head movement provokes symptoms. Dr. Campanella likes to ask if symptoms come on when you tilt your head back like when you get your hair washed. The more severe the vertigo, the more likely it is peripheral vertigo. Peripheral vertigo is more common in women. Usually occurs in the 4th-5th decade.
Halpike testing is specific for peripheral vertigo. There is latency of the effects of this test though so you have to wait for up to a minute to see if patient has symptoms. The otoliths are floating in the endolymph and it takes some time for them to stimulate the hairs in the semi-circular canals.
Meniere’s: There is an over-accumulation of endolymph within the vestibular system. Patients have vertigo and hearing loss over time. The other name for meniere’s is Otolithic Catastrophes of Tumarkin. True name but we all got a good laugh from it.
Any type of dizziness may worsen with positional change but only peripheral vertigo results from position change.
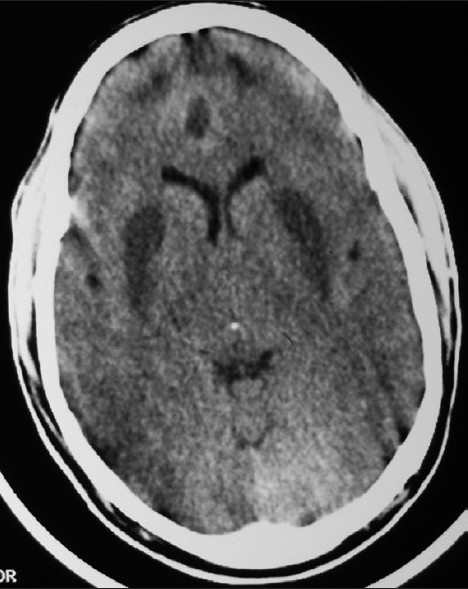
Thinking about stroke localization: When you are dealing with the D’s (dystharthria, dysphonia, dysphagia, diplopia, dizziness, dysequilibrium) you are talking about stroke in the posterior fossa.
Migraines can cause vertigo. Don’t give these patients (specifically migraine induced vertigo) tryptans for their headache because you can cause vasospastic stroke.
Wallenberg syndrome: Also known as the lateral medullary syndrome. Symptoms include:hoarse voice, horner’s syndrome, nausea, facial numbness, blurred vision/diplopia, difficulty standing unassisted, limb ataxia and vertigo. This is a stroke but these patients have no extremity weakness so it is a tricky diagnosis. It is a stroke affecting the lateral medulla and is due to Posterior Inferior Cerebellar Artery which is a branch off the vertebral artery.
Campanella does not use the head impulse test to evaluate vertigo. He doesn’t find it useful

*Wallenberg Syndrome
Campanella did not have clear age cut off for who he would scan. He discusses the decision to scan with the patient. He feels that if history/physical is pretty clear cut for peripheral vertigo and pt can walk and is not sick from vomiting they can be discharged. If you see any previous stroke on CT that suggests that this patient’s symptoms are due to a cerebrovascular event based on signs of previous stroke.
Elise comment: Should we pass on CT and go right to MRI for dizzy patients? Campanella: Sure, if you can get it done it does possibly save an admit for the patient and speed up the evaluation.
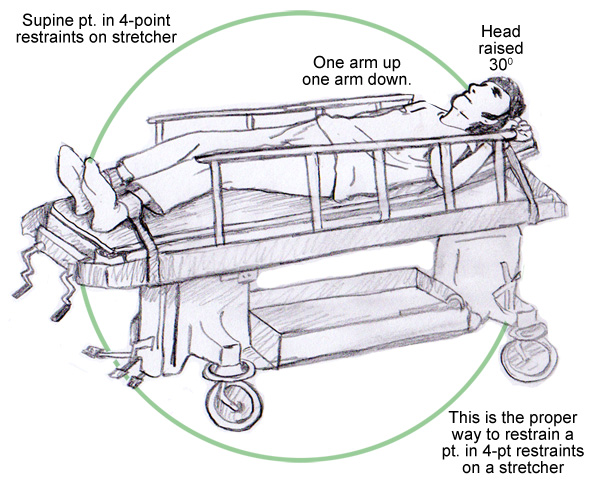
Girzadas Airway Management of the Morbidly Obese Patient
Since I gave the lecture, I did not take notes but the key take home points are listed.
Obese patients have rapid desaturation when apneic due to a decreased functional residual capacity and overall diminished lung function as well as increased utilization of oxygen. More rapid desaturation reduces the safe apnea period that emergency physicians have to secure an airway.
Obese patients have more difficult visualization of their airway. They also have increased risk of aspiration.
Strategies to mitigate the above pathophysiology include
Preoxygenation with head up at 20-30 degrees.
Passive oxygenation with 15 L per nasal cannula during preoxygenation and during intubation.
Preoxygenate with 15L NRB mask with O2 cranked above 15 L per min
If this is unable to get O2 saturation above 95% use bipap.
While preoxygenating patient put patient in RAMP position to optimize airway visualization.

Suggested approach to intubation is Ketamine sedation with topical anesthetic in the upper airway and not do RSI if possible.
Video laryngoscopy should be your first attempt device based on research showing VL gives better visualization and shorter intubation time in obese patients.
Go-to Rescue device should be intubating LMA.
If you need to cric, don’t delay as these patients desaturate rapidly and cricothyrotomy in the obese patient takes more time. Use an ET tube instead of a shiley to give yourself more length to reach the airway.
Estimate drug doses based on body weight of 100kg.
Settings on the ventilator should be based on ideal body weight and low tidal volumes. 70 kg and TV of 6ml/KG. So TV of 450-550 is a reasonable starting point.
Remke 5 Slide Follow Up
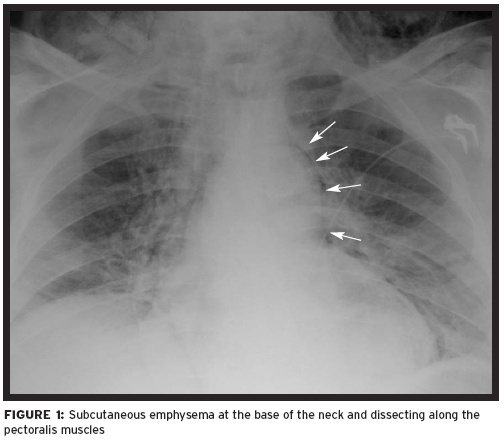
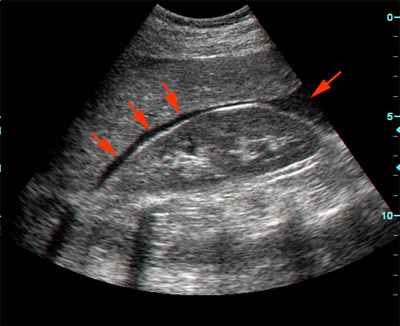
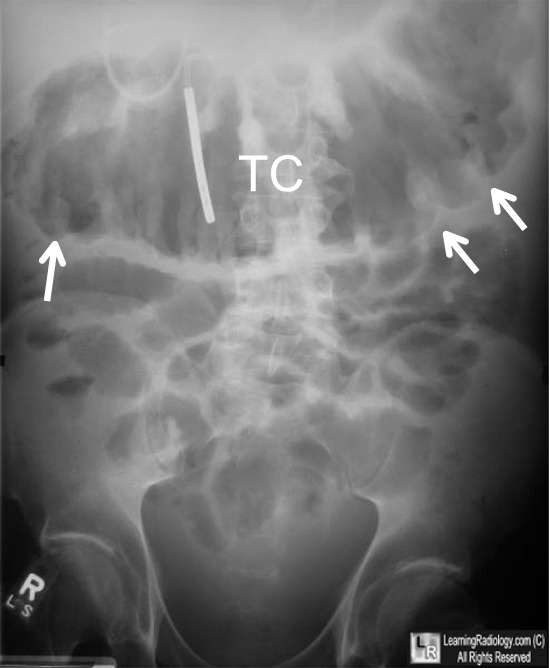
Pt has trauma to her lower leg. The ED physicians have suspicion of compartment syndrome. Patient has a history of bilateral PE and is on warfarin.
Compartment syndrome is due to an increase in pressure within a muscle compartment bound by fascia. Diagnosis is based predominantly on pain out of proportion of exam and tense compartments. 5 P’s Pain, Pulse deficit, Pallor, Paresthesia, Paralysis. Compartment measurement that is within 30mm of Hg of the diastolic blood pressure should go to the OR.
Decision was made to reverse coagulopathy with FEIBA and patient went to OR for fasciotomy. After fasiotomy patient was anticoagulated pretty much right after surgery.
Navarrete 5 Slide Follow Up
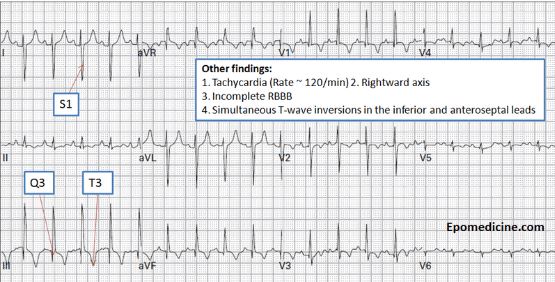
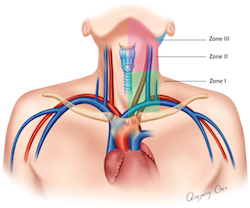
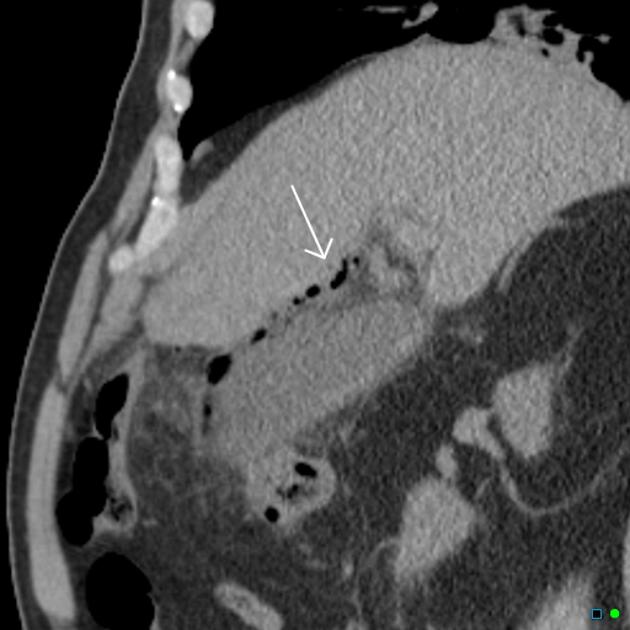
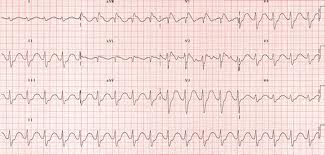
31yo male with acute right leg numbness. Patient had a fever and cough for the last several days. No chest pain. Patient did have diminished pulses in the right leg.
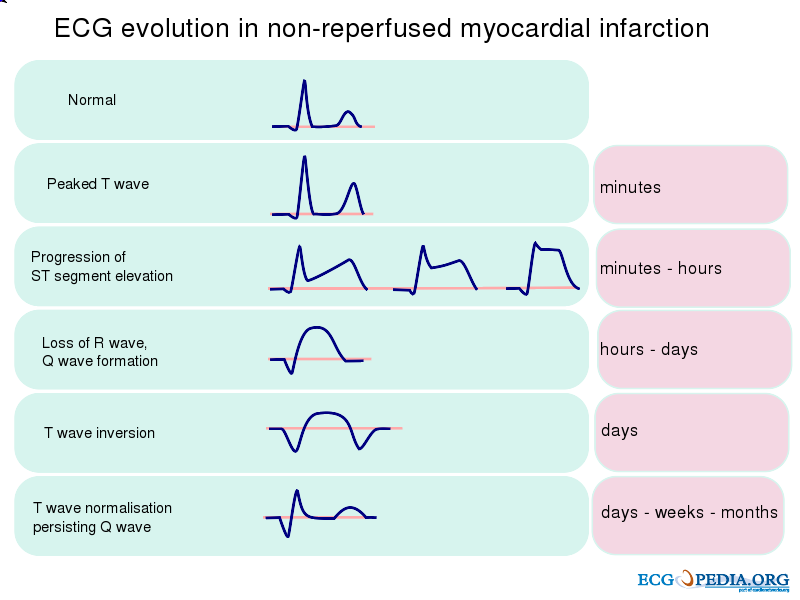
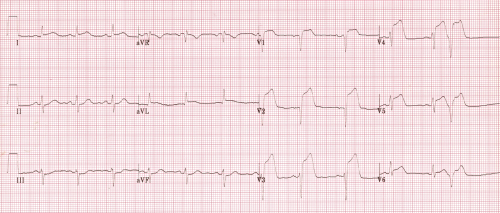
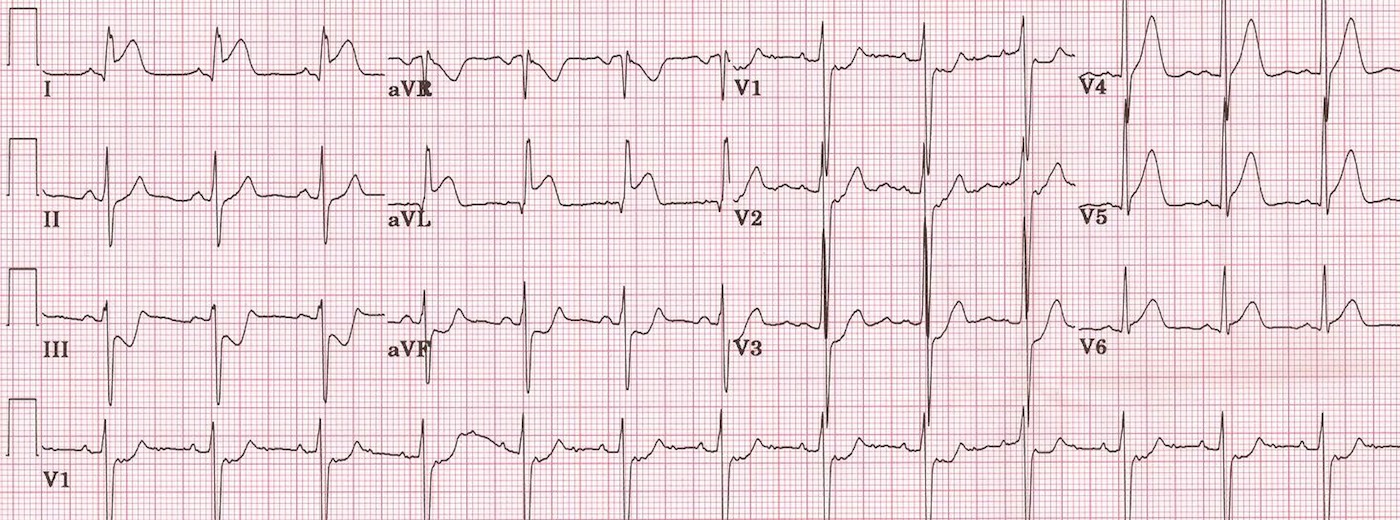
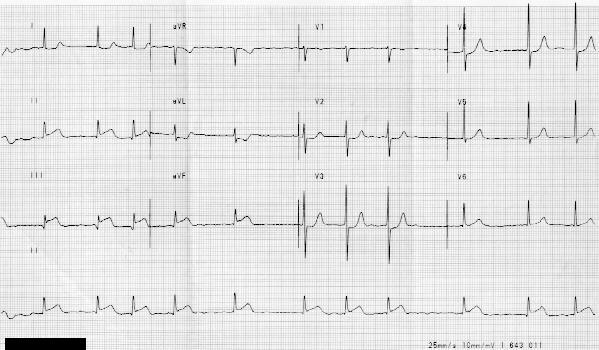
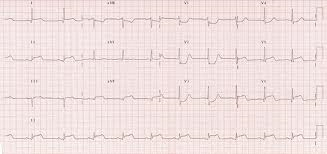
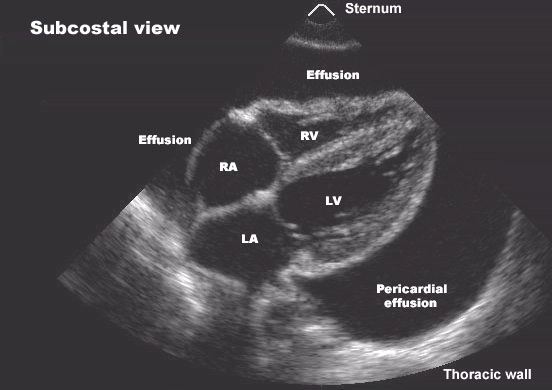
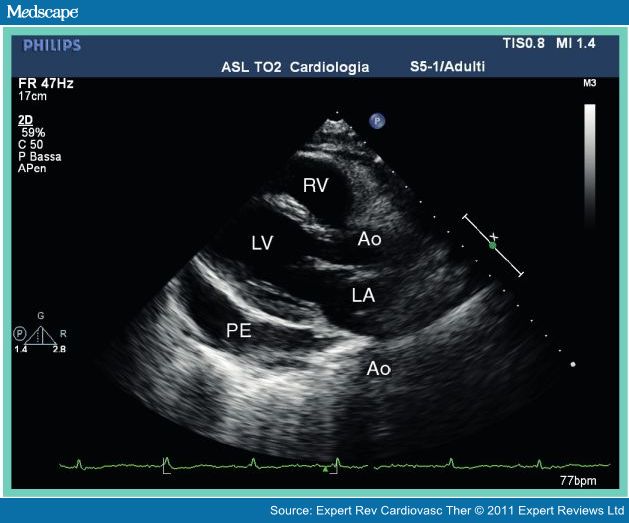
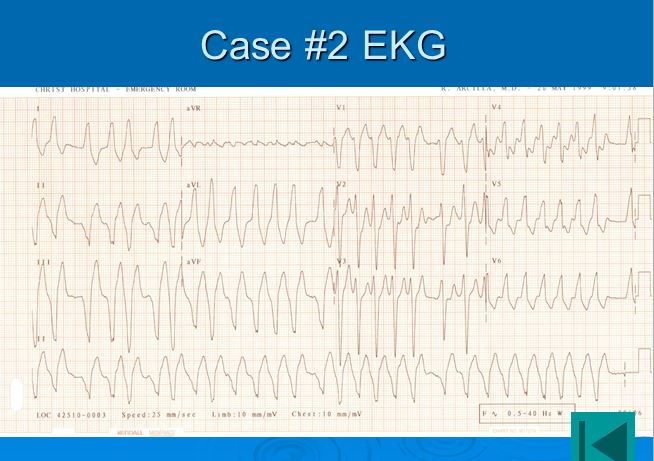
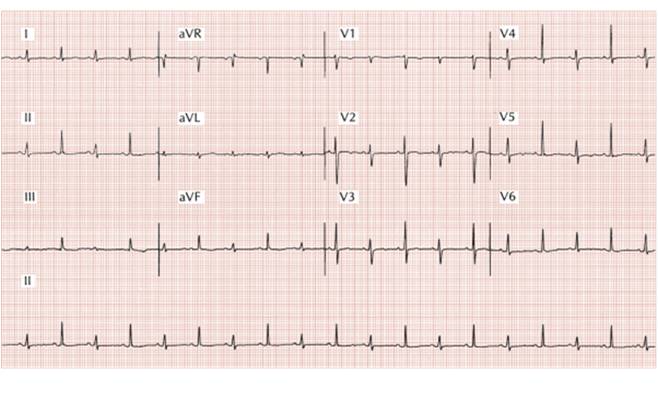
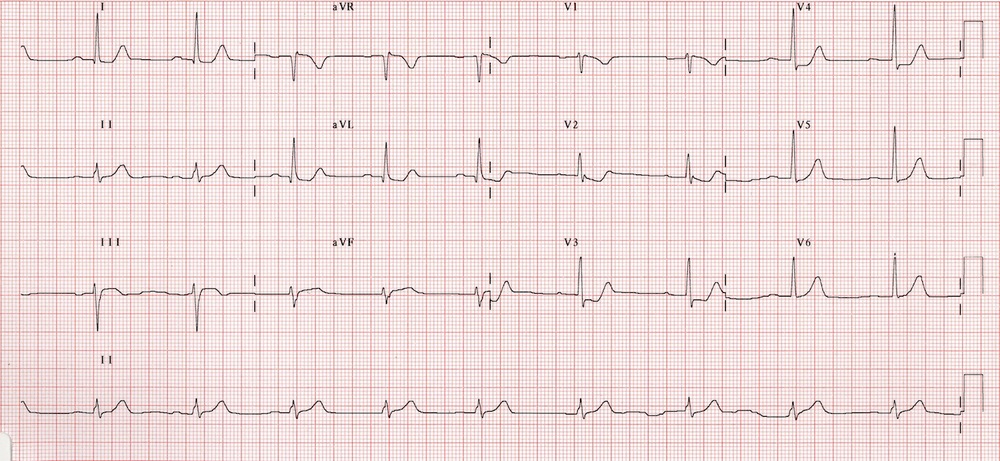
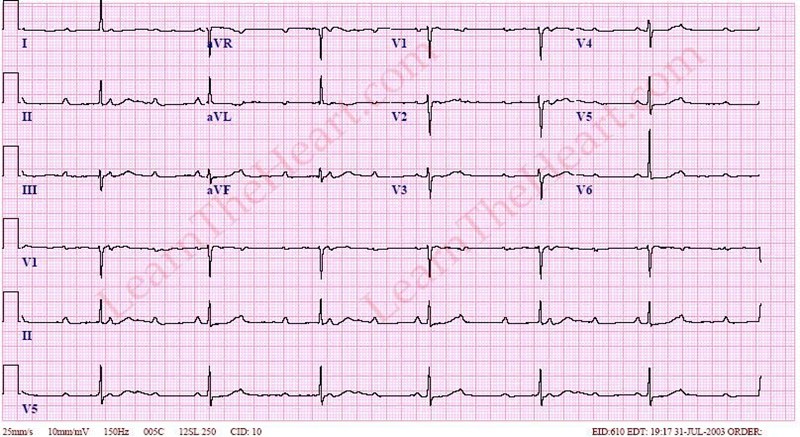
Ekg showed sinus tach. WBC=24.5. Troponin=1.21. Diagnosis in the ED was endocarditis. Formal TEE showed a vegetation on the aortic valve. CTA showed thrombus in the right common femoral artery and infarcts in the spleen and left kidney. Patient seemed to become more ill in the ED but was still overall stable so he was sent up to the ICU. 3 hours later in the ICU the patient arrests. He was found to have an acutely blown aortic valve. Patient was resuscitated and taken to the OR. He survived.
If you identify an ischemic limb, you gotta think clot, endocarditis, AND dissection.
You can use ABI’s to objectively verify your exam. >0.9 is normal. <0.5 is a severe occlusion.
Treatment for clotted vessel is heparin bolus and drip. Consult vascular surgery. CTA is recommended for imaging the suspected vascular area in the ED.