Permar M&M
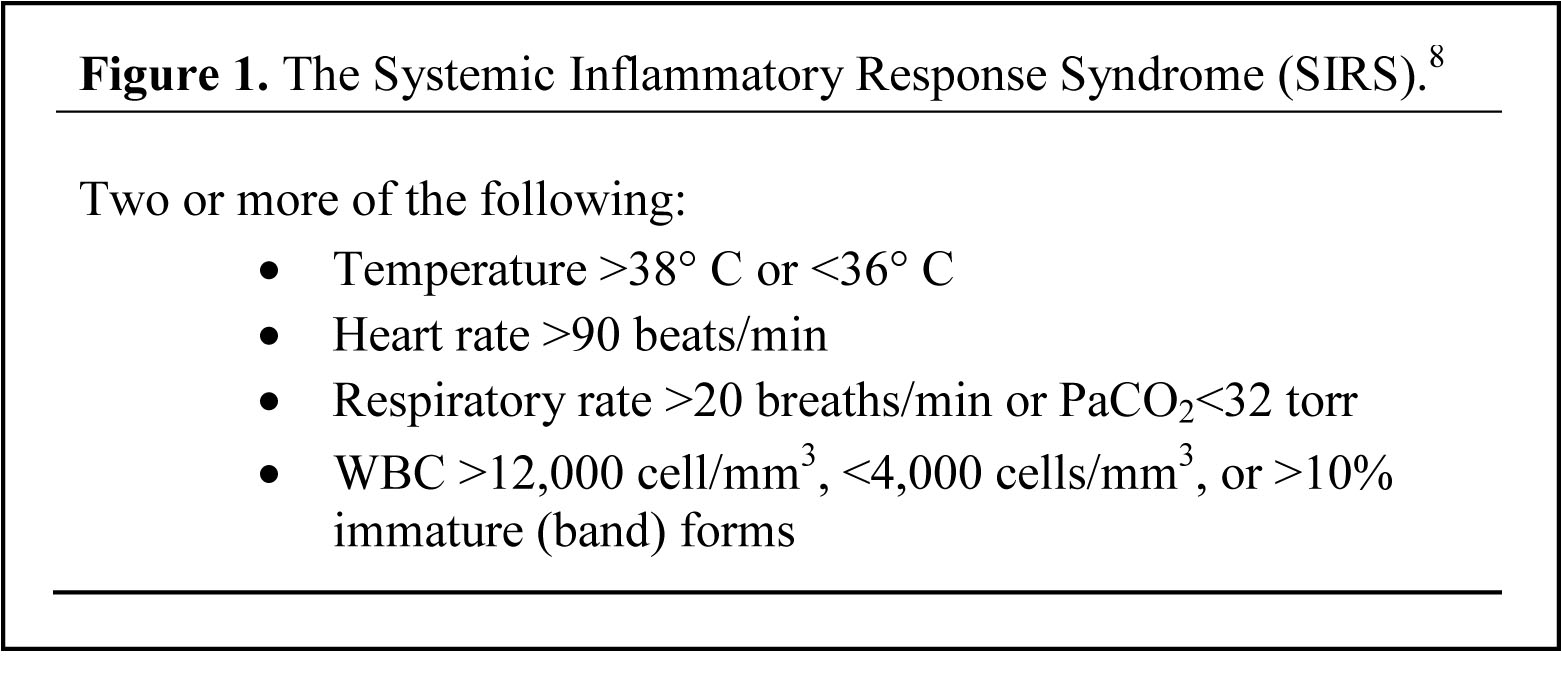
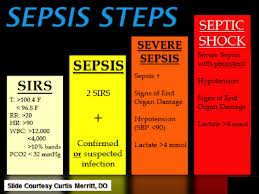
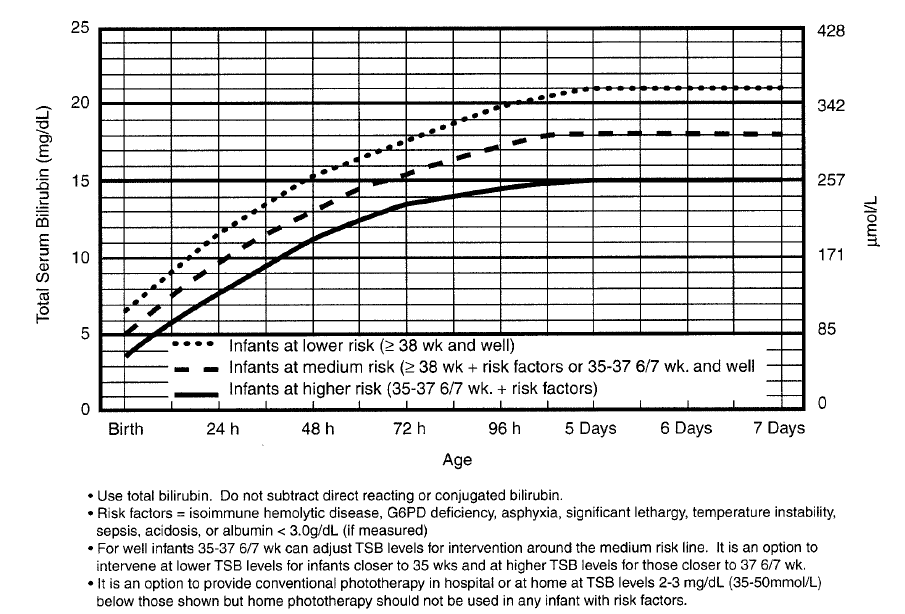
9 day old female born at 38 weeks without complication. Patient presents with jaundice, decreased PO intake, no fever. T=37.2, HR=113, RR=26, BP=81/52, SPO2=100%
Patient noted to be lethargic. Mucosa was somewhat dry. Bilirubin level was ordered by the resident.
Attending saw the patient and advised that a septic workup should be done.
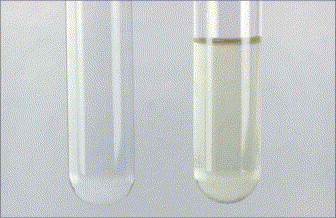
When labs come back, the total bili was 28! LP was performed and showed CSF fluid that was yellow tinged due to elevated bilirubin.
The Pediatric service advised PICU admission for management of the bilirubin level and possible exchange transfusion.
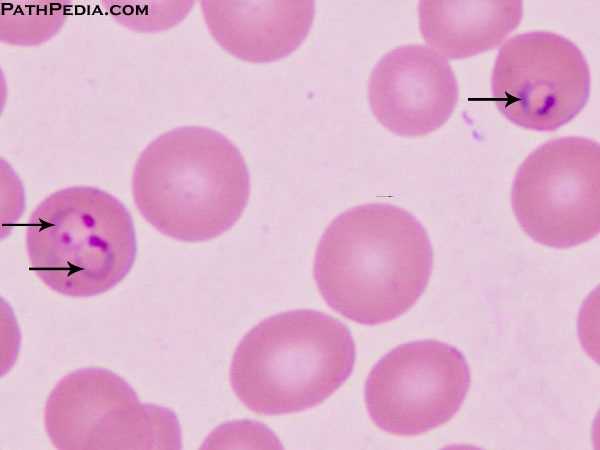
Elevated bilirubin develops from increased fetal HGB breakdown. Neonatal hepatic function is slow compared to older infants and adults. By 14 days of age, most neonates have reached adult level hepatic function and in most infants neonatal jaundice is resolved by that time.

*Bilirubin Metabolism (Colletti EM Clinic Nov. 2007)
Causes of indirect (unconjugated) hyperbilirubinemia: physiologic jaundice, ABO incompatability, sepsis, cephalohematoma, enzyme deficits. Breast milk jaundice is the persistence of physiologic jaundice beyond one week. Human milk promotes bilirubin absorption in the gut. Breast feeding failure jaundice results from lactation failure and inadequate fluid intake. Hypovolemia results in elevated bili levels and increased enterophepatic reabsorption.
The problem: Bilrubin crosses the blood brain barrier and can cause damage to the basal ganglia, hippocampus, and cerebellum, and some cranial nerves. BIND=B=bilirubin I=Induced N=Neurologic D=Dysfunction. Patients with BIND can have hypotonia/hypertonia, decreased alertness, poor feeding and develop long term cognitive deficits.
Danger signs in the Jaundiced Neonate
1. Family history of significant hemolytic disease
2. Vomiting
3. Lethargy
4. Poor feeding
5. Fever
6. Onset of jaundice after the third day of life
7. High-pitched cry
8. Dark urine
9. Light stools
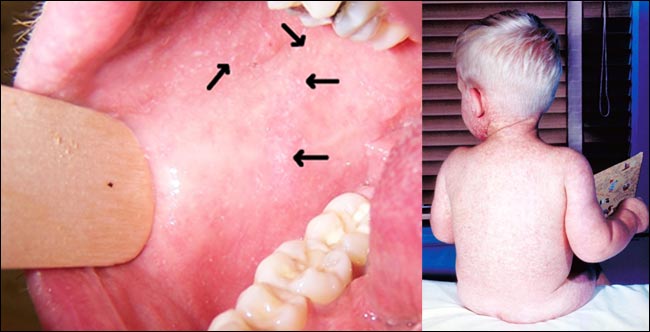
Galactosemia presents as feeding intolerance manifested by persistent vomiting, an
enlarged liver, seizures, and lethargy. Ill appearing patients will likely be acidotic. Newborn screening should pick this up, but there can be false negatives.
In a well-appearing, afebrile infant with unconjugated
hyperbilirubinemia and normal hemoglobin, no further tests are needed.
Conjugated hyperbilirubinemia is concerning because, although it is nontoxic,
it is a marker for serious underlying disease. Associated findings of conjugated
hyperbilirubinemia are pale acholic stools, dark urine, or the presence
of bilirubin in the urine. (Colletti EM Clinic Nov. 2007)
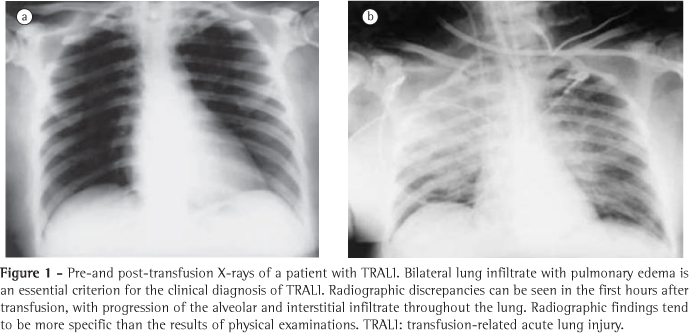
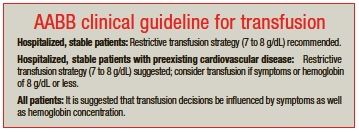
The mainstay of treatment for hyperbilirubinemia is phototherapy. Modalities beyond phototherapy include IVIG and exchange transfusion. Exchange transfusion has the usual risks associated with transfusions.
Take home lessons:
Be alert for the sick neonate
Consider sepsis in every jaundiced neonate
Be alert for delays in how your work up was going.
Get phototherapy started as soon as possible after identifying a bilirubin >18.
In severely high bilirubin levels (>25) consider IVIG and/or exchange transfusion.
Harwood comment: What was the discharge diagnosis? Trale: Breast feeding failure jaundice. Elise comment: What are the patient safety concerns of phototherapy? Trale: Infants need eye protection and you have to avoid overheating the infant or causing a skin burn. Erik comment: Consenting parents to do an LP may unnecessarily delay care. Girzadas comment: You have to consider sepsis as a differential diagnosis in every jaundiced neonate. You don’t have to work up every jaundiced infant for sepsis but you at least have to consider and rule out that diagnosis in your head before moving on to treatment. The fact that you saw bilirubin in the CSF really demonstrates the idea that the brain is being bathed in bilirubin and you need to act rapidly to get that level down.
Carlson Study Guide Toxicology
Pepto-Bismal, Ben-Gay, and wart removers contain salicylate. The pediatric formulation of pepto-bismal has no salicylate to avoid causing Reye’s syndrome.
If a toddler ingested or is suspected to have ingested a sustained release calcium channel blocker they need to be admitted and observed for over 12 hours. Children with this overdose have been reported to crump 12-18 hours after ingestion even though they looked well initially.
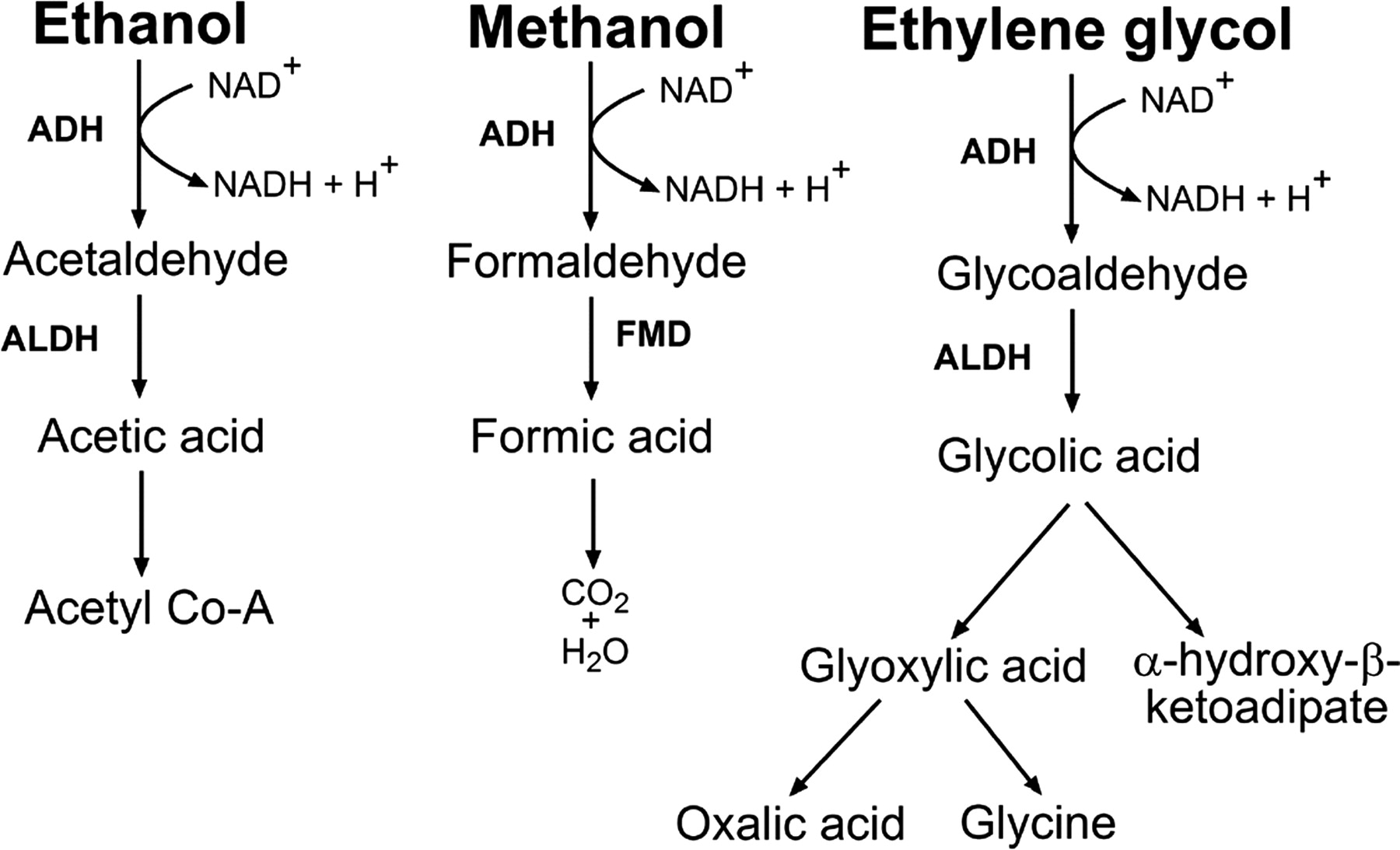
NAC works as an antidote for APAP by increasing glutathione supply, detoxification of NAPQI and enhance hepatic microvascular function.
*NAC for Acetaminophen Poisoning
14 yo female reports an ingestion of 10g of APAP 45 minutes ago. Best management? Answer: Give activated charcoal and wait to get a 4 hour APAP level. If the 4 hour level is over the possibly toxic line (150 at 4 hours), give NAC. As long as NAC treatment is started within 8 hours, patients universally do fine.

*Rumack Matthews Nomogram for Acetaminophen Poisoning
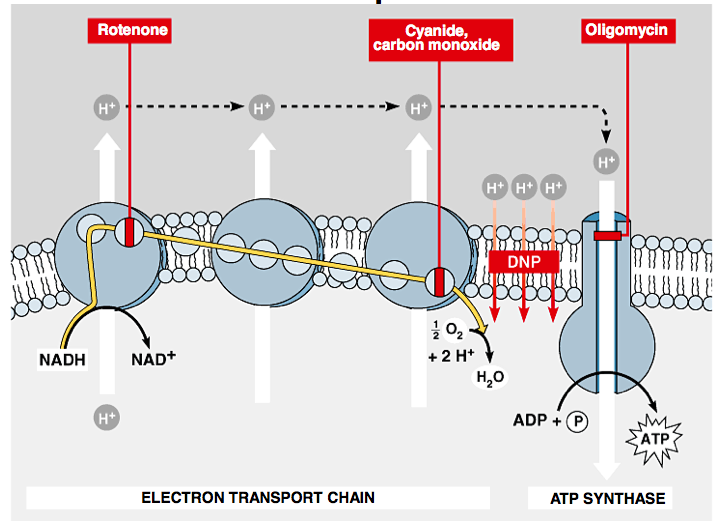
Glucagon is used in beta blocker toxicity to increase cAMP in order to increase cardiac contractility.
Verapamil is the most common cause of death among calcium channel blocker overdoses due to having both strong smooth muscle relaxation effects and strong AV nodal blocking effects. These patients get both hypotensive and bradycardic.
Caffeine acts on the adenosine receptor. If a patient has a caffeine overdose, lower doses of adenosine may not work to control SVT. You may have to use higher doses of adenosine (12-18mg)or choose a beta blocker (like esmolol or metoprolol) or cardioversion instead to get the patient back into sinus rhythm.
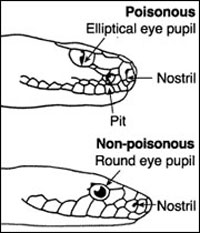
Digoxin-like plants include oleander, foxglove, and lilly of the valley.

*Oleander
Jimson weed has anticholinergic effects.

*Jimson Weed
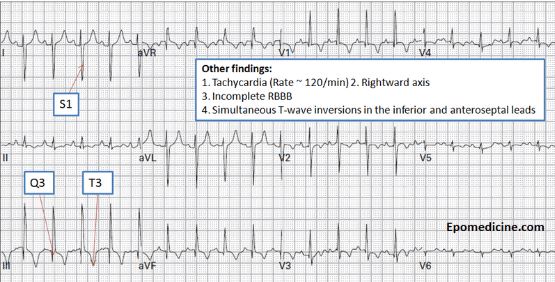
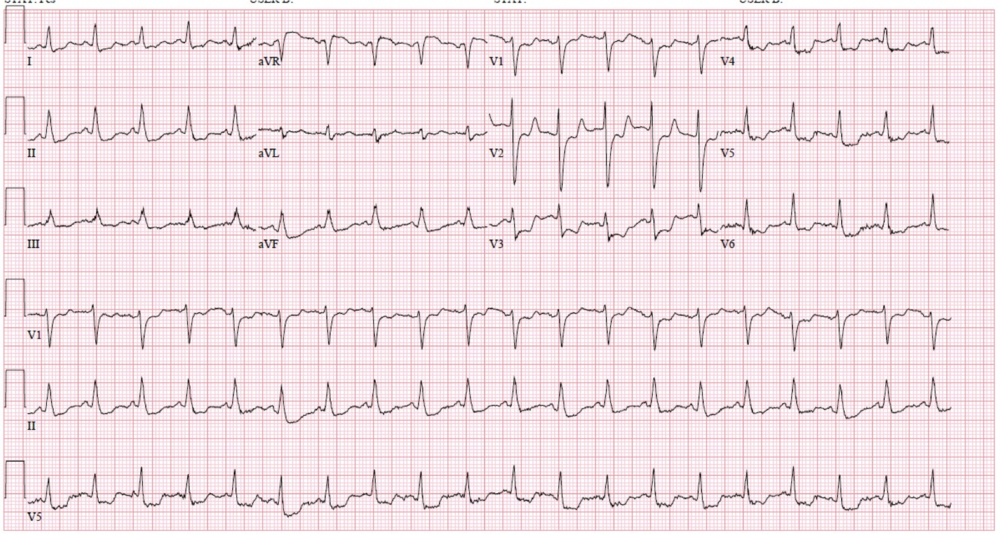
Sotalol is possibly the most common prescription drug cause of torsades
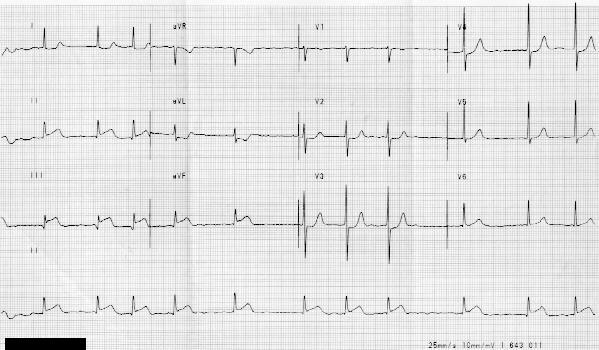
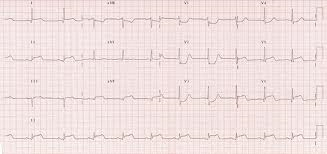
 *Torsades
*Torsades
Patients with high phenytoin levels are at risk for falling due to ataxia. Phenytoin does not cause primary cardiovascular instability or coma. Consequently if you admit a patient with phenytoin overdose, you are admitting them to protect them from a fall. They don’t need the ICU or Tele because arrhythmias and coma are not a concern from this overdose.
Morning glory plant seeds have LSD-like substances in them. If you buy them in the store, manufacturers add an emetic substance so if people try to eat them to get high they will instead vomit.
Insulin acts in CCB poisoining to increase myocardial glucose uptake. It works to alleviate the “starving myocyte” in CCB poisoning.

*Starving myocyte in Calcium Channel Blocker and Beta blocker poisoning. Insulin acts to increase intracellular glucose. Glucagon acts to increase intracellular cAMP.
High dose glucagon infusions for B-blocker toxicity may cause nausea and vomiting.
The biggest benefit of fosphenytoin over phenytoin is that it can be given IM.
Most common lab test abnormality in theophylline overdose is hypokalemia.
Dextromethorophan and Ketamine can cause a positive result for PCP on urine drug screen.
Neal Lyons Pharmacist Lecture on ED Protocols
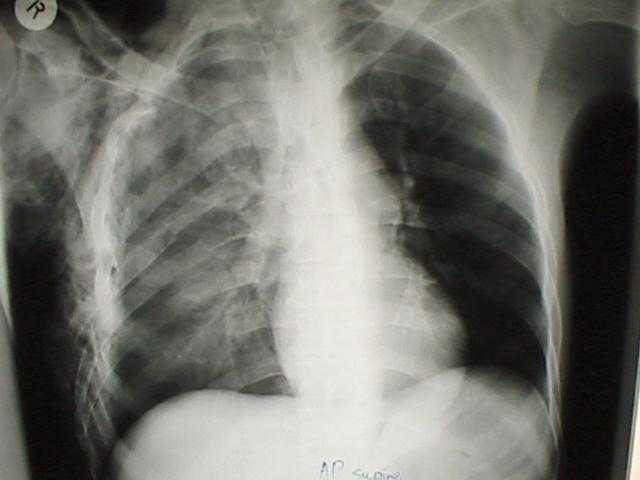
65yo male on ventilator for flash pulmonary edema. Best sedation medication is fentanyl. Harwood comment: As long as they are intubated, hit them hard with fentanyl so they are calm. Give 50-100micrograms and keep the drip at about 50 micrograms/hour. If fentanyl is not effective add benzodiazepines or propofol.
65 yo male with severe ETOH withdrawl. Start with IV Ativan 8mg Q15 minutes X 5 doses. If still not under control, then move on to phenobarbital 260mg IV. Then start Ativan infusion at 10mg/hr. Next give phenobarbital 130mg IVP Q 15 minutes up to 8 doses. Elise comment: Is it ok to just load the patient with 1300mg of phenobarbital up front with a drip instead of 130mg aliquots? Neal: Yes definitely.
Max dosing of Ativan is 30mg/hr. By this time patient will likely be intubated. If patient still not controlled, IV propofol is started.
Htet comment: There is some research in the ICU describing the use of ketamine for severe ETOH withdrawl. Neal: Yes that is correct. I am skeptical about using ketamine for severe alcohol withdrawl, but we’ll see. Another option may be dexmedetomidine, but it’s use is very restricted at our institution. Ketamine and dexmedetomidine act at a non-GABA sites. Ketamine works at the NMDA receptor and dexmedetomidine works in the locus ceruleus. So there is some logic to using these drugs if GABA-acting drugs like benzo’s and Phenobarbital are not controlling the patient.
Harwood comment: Despite these major doses of benzo’s and phenobarbital, alcohol withdrawal patients are so adrenergic ally revved up they may not have severe respiratory depression to require intubation. They are different than say seizure patients who get benzo’s and phenobarbital and have marked respiratory depression with high doses of the same drugs.
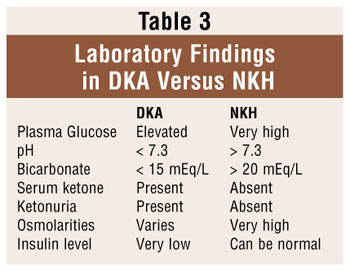
25yo patient in DKA. Give 1.5 maintenance rate of IV fluids. No IV fluid bolus unless patient is in shock. Neal says 20meq of KCL /hour through a peripheral line is OK. You can go over the soft limit of 10meg KCL per hour if needed to manage hypokalemia in the DKA patient. Elise comment: Don’t give insulin boluses either. Just start a drip 0.1u/kg/hour. Harwood comment: I am sad that bicarb is still on the protocol. You don’t need bicarb for DKA unless you are doing CPR on the patient. When managing the DKA patient, the goal glucose level is 250. The goal rate of glucose decrease is 50-100mg/dL/hr. Elise comment: Please make sure you know the potassium level is in the normal range before starting insulin. Be aggressive to supplement potassium while the patient is on an insulin drip.
Navarrete comment: Really try to avoid stopping the insulin drip as the sugar gets into the 200’s/100’s. Instead of turning the insulin drip off, decrease the drip to 1u/hour. You should be able to maintain a reasonable blood sugar while at the same time continuing to clear acidosis and not risking a raid bump back up in blood sugar if you turn the drip off.
65 yo male with ICH due to warfarin use. Give FEIBA 500 units and vitamin K 10mg IVPB. Recheck INR in 30 minutes. If INR is less than 1.5 no further intervention is indicated. If INR is still >/= to 1.5 consider another dose of FEIBA 500 units. Elise comment: FEIBA is only for life threatening bleeding. There is a significant incidence of clotting complications with this drug. It is too dangerous to be used for more minor bleeds. If a patient has life-threatening bleeding due to rivaroxiban, they get a much higher dose of FEIBA. Give 50u/KG of FEIBA. This works out to 3500units for the 70kg lean body weight patient. This is similar to hemophilia type dosing. Vitamin K has no added benefit is bleeding due to rivaroxiban.
West Cost Effective Lab Testing
Limit magnesium testing to: Patients with arrhythmias, low Calcium, refractory low potassium, muscle irritability/tetanus. Consider magnesium testing for: Patient with chronic diarrhea, PPI usage, diuretic usage, alcoholism, and renal disease.
Limit coagulation testing to patients with liver disease, impaired clotting, those taking anticoagulants, or based on history or physical exam showing bleeding tendency or risk.
No need to ever order CK-MB when evaluating patients for suspected cardiac disease. Troponin is superior in all circumstances to pick up infarction and re-infarction.
Navarrete Hyperemesis Gravidarum
>50% of pregnant women will have nausea. Usually nausea starts around 4 weeks EGA.
Early pregnancy symptoms: nausea and vomiting, food aversions, fatigue, increased saliva, sensitivity to smell, constipation, and heart burn.
There is a link between hyperemesis and H Pylori.
An increased incidence of infection with Helicobacter pylori has been observed in
women with HG and is now considered to play a role in its pathogenesis. Frigo and
colleagues59 found that 90.5% of women with HG were H pylori IgG positive,
compared with 46.5% of controls. Bagis and colleagues60 used the gold standard
test, histologic examination of the mucosal biopsy, and found that 95% of HG patients
tested positive for H pylori compared with 50% of controls. These investigators also
found higher H pylori densities in the gastric antrum and corpus in HG patients, suggesting
a possible relationship between H pylori density and the severity of symptoms.
A systematic review from 2007 evaluating 14 case-control trials from 1966 to 2007
found a significant association between maternal H pylori infection and HG in 10
studies. Odds ratios in the studies varied from 0.55 to 109.33.61 Similarly, an updated
systematic review and meta-analysis from 2009 of 25 studies found a pooled odds
ratio of 3.32 (95% CI: 2.25–4.90) for H pylori infection in women with HG.62 Of note,
high heterogeneity among studies was found in both reviews.
Infection with H pylori in pregnancy may occur because of steroid hormone–induced
changes in gastric pH63 and/or increased susceptibility due to changes in humoral and
cell-mediated immunity.64 However, there is no clear evidence that pregnancy predisposes
to de novo H pylori infection. On the contrary, it has been suggested that H
pylori may exacerbate hormone-induced changes in the nerve and electric functioning
of the stomach, and thereby increase the risk for infected women to be at the more
severe end of the spectrum of nausea and vomiting.61 (Lee, Saha. GI Clinics of NA June 2011)
Hyperemesis is defined by dehydration, 5% weight loss, or electrolyte abnormalities.
General early measures: small meals, eat small bites, cold/carbonated/clear fluids, take prenatal vitamins at night with a snack, drink fluids 30min before and after meals instead of with meals to decrease stomach distension, and protein intake may decrease nausea.
Complimentary medicine: acupuncture, acupressure, hypnosis, and ginger tea may be of value.
Medications: Diclegis is the combo of pyridoxine 10 mg and doxylamine 10mg. Pregnancy Categorgy A. It is somewhat expensive. The same combination years ago was called bendectin which was taken off the market in 1983 due to concerns and lawsuits about birth defects. Re-evaluation of the data has shown that pyridoxine and doxylamine do not cause birth defects. So you can prescribe diclegis or tell mom to buy vitamin B 6 pills and unisom (doxylamine) as a cheap over the counter alternative to diclegis.
ED treatments: Reglan can be used but in 33% of women it causes movement disorders. Zofran can be used. It is considered safe. Elise comment: Recent big epidemiologic study on Zofran from Denmark showed it was safe. Also the OB faculty are OK with Zofran if B6/doxylamine are not working.
Start with an 8mg dose of zofran. Zantac and Pepcid OK for heartburn( both are Pregnancy Category B). IV fluids 0.9 bolus and switch to D5.45 as a maintenance fluid.
Harwood comment: I’m starting with B6 25mg/doxylamine 10mg first line. My second line based on the most recent data would be Zofran 8mg IV.
E Kulstad Adasuve (Loxapine) Antipsychotic Medication Research Trial for ED Use
This drug is a typical antipsychotic indicated for acute treatment of agitation associated with schizophrenia and bipolar disorder. It is an inhaled formulation.
There have been some incidences of bronchospasm in treated patients.
Not indicated for severely agitated patients requiring restraint. Patients have to be cooperative to take the medication. They have to inhale the drug on their own.
Can’t be used in patients actively wheezing.
Patients have to be monitored for bronchospasm. They need lung auscultation every 15 minutes for at least an hour.
Elise comment: The cost is much higher than Geodon/Ativan
Girzadas questions: Does the patient need a prior diagnosis of schizophrenia or bipolar disorder to receive the drug? Erik’s response: They don’t need a documented prior diagnosis. Girzadas question: How much bronchospasm can they get? Erik’s response: It has been infrequent and has been mild. It is contra-indicated in patients with asthma, wheezing, or COPD.
Harwood comment: It seems strange they are not marketing this drug as an oral dissolvable tablet.