Much Thanks to Christine and Elise for keeping the Conference Notes going while I was down in Australia!
Joint EM-Peds Conference M&M
5 week old female. 4 week hx of diarrhea. PMD tried multiple formula changes. On arrival to ED, pt not taking po and appears dry and pale/grey. Also grunting noted. IV placed expeditiously and fluid bolus given. Unable to obtain labs initially. Sign out occurred at this point. Further attempts at obtaining labs failed. Finally ,via 4 heel sticks, labs were obtained. K=7.9 and HCO3<5. Re-eval of child showed ill but non-toxic appearance. Parents refused further attempts at blood draw. Pt was transferred to the floor at this point. On floor, skin was cool/pale, pt still grunting, HR=146. PICU came to evaluate patient on floor and found pt to be lethargic and gray in color. ABG showed a ph<6.8. MetHGB=33%. Pt was intubated, septic work up performed, methylene blue was given. Pt did well. Pt had a congenital food protein related methemoglobinemia.
Issues: There was early recognition of the sick child. There was difficulty obtaining labs. Handoffs were considered less than optimal in that severity of illness and management algorithm was not completely clear to receiving teams. Interdepartmental communication may have been suboptimal. PICU team was not involved in this case while patient was still in ED. Bedside handoff may have been helpful to improve the clarity of clinical communication between teams.
Positives: Rapid IV access was obtained. Multiple re-assessments were made of the patient by the receiving teams in the ED and on the floor. There was very good communication with the patient’s parents. Early recognition/treatment of methemoglobinemia and transfer to PICU.
Kettaneh comment: Optimally PICU could have been consulted prior to the first sign out. It is helpful to give a management algorithm based on diagnostic testing results to the receiving team.
Roy comment: It is great that the patient was re-evaluated multiple times in ED. Also very positive that methemoglobinemia was identified and treated rapidly.
Harwood comment: There are multiple system issues. This case involved multiple fatigued docs signing out to other fatigued docs. ABG was a critical test in this case. It is good that MetHGB is part of the ABG panel. If you are facing difficulty getting labs in a seriously ill child, you can get labs from IO draws (T&C, Glucose, Cr, HCO3 are all valid).
Roy comment: I agree ABG was very important. Just thinking of alternative diagnoses, if this patient had a high bicarb on ABG it would make CF very likely.
Suggestions for system improvement: C. Kulstad comment: ER physicians should not be defensive toward Peds Resident suggestions when discussing tranfers of care. Both teams should discuss options in difficult cases. Notario comment: Bedside rounding would have been helpful to get fresh eyes on the patient.
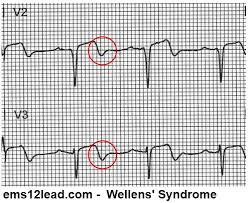
Herrmann/Kettaneh STEMI Conference
Case 1. Chest pain resolved prior to arrival in ED. Inital EKG was non-specific. Possibly some Wellens changes anteriorly. E. Kulstad, Cardiology comments: Wellen’s is not a criteria for Code STEMI but cardiology should be consulted for non-emergent cath the same day. 2nd EKG with no pain shows Wellen’s signs. Cards consulted. Trop was 0.07. Pt was cathed later that day. Pt had an 80% lesion of LAD that was stented. There was a discussion of the timing of Cath in Wellen’s patients. General agreement that these patients don’t require emergent catheterization if pain free. Ok to start ntg and beta blockers and anti-platelet therapy and arrange prompt cath (12-24 hours). Wellen’s changes are usually noted when pt is pain free. With chest pain, the changes normalize or evolve to STEMI. Post-cath, the EKG in this patient normalized. Al-Kaled comment: Wellen’s syndrome includes chest pain. If you see these findings in an asymptomatic patient, technically it is not Wellen’s syndrome.
Wellen’s EKG
Case 2. Ekg showed Afib with anterior Q waves. Minimal ST elevation noted in lead 3 and minimal ST depression 1 and AVL. Cardiology consensus was that this was not an acute STEMI. 2nd EKG was similar. 3rd EKG now has minimal ST elevation in AVF and possibly more ST depression in 1 and AVL. 4th EKG has ST elevation in 3 and AVF. STEMI was called on 4th EKG. Cath showed no coronary artery disease but pt had embolism to distal LAD due to Afib. There was much disagreement among cardiologists present about the management of this patient. Most agreed that patient had to go to cath lab with ongoing pain and worsening EKG. Cardiologists made the point that taking the very elderly to cath is treacherous and if at all possible, attempting a short trial of medical management on elderly patients without screaming STEMI findings on EKG may be prudent before pulling the trigger on a Code STEMI. Afib with embolus to the coronary artery is relatively rare. Mechanical valves can also shower emboli to coronary arteries. Cardiologists note that patient can have concurrent emboli to heart and brain or heart and gut.
Case 3-5. Multiple rapid fire EKG’s presented. There was a case of a patient with sob and anterior horizontal ST depression with associated ST depression in AVR. Most cardiologists would call a STEMI based on that EKG for posterior MI. Posterior leads showed minimal ST elevation in Post V4 and V5 leads. Cath showed Circumflex lesion.
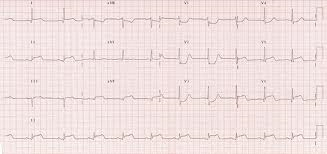
Posterior MI
Last EKG was in a DKA patient. Silverman comment: Use Echo in a young patient. If the anterior wall is going like gangbusters it is not going to be a STEMI.
Permar Trauma Lecture
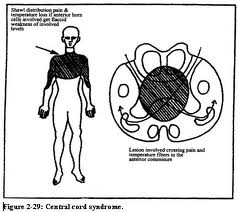
60yo Male fell out of a tree. No sensation below nipples. Could not move upper extremities. Pt is hypotensive with borderline bradycardia. Diagnosis: Central cord injury of cervical spinal cord.
Spinal cord injuries are most common in young adult males. 47% are due to MVC’s. ETOH and underlying spinal disease increase the risk. Most (55%) Cord injuries involve the cervical spine.
Primary injury= Immediate effect of trauma. Secondary injury= Progressive injury following initial traumatic insult (ischemia, hypoxia, inflammation, edema, apoptosis)
Backboards can cause pain and their benefit is unproven. They are the standard of care however in the US.
NEXUS Criteria

Canadian C-Spine Rule
Flexion-Extension views may pick up a ligamentous injury. 30% are non-diagnostic. Omi comment: For patients with persistent pain this is a worthwhile test to rule out ligamentous injury. It may save the patient and MRI. Most useful in a younger, thin patient. Bigger or more muscular patients will have very limited images and MRI is more useful for these patients.
Unstable Cspine Fractures: mnemonic: Jefferson Bit off A Hangman’s Thumb. Jefferson Fx, Bilateral Facet dislocation, Odontoid fractures, Atlanto-axial dislocation, Hangman’s fracture, Teardrop fractures.
Back to case: Pt had bilateral C1 arch fractures with central cord syndrome.
Central cord lesion: Due to forced hyperextension injury.
Anterior Cord Syndrome: Commonly due to Disc herniation or bone fragmants.

Brown Sequard: Due to penetrating injury to Cord.

Neurogenic shock: Hypotension and bradycardia. Due to interruption of autonomic pathways causing decreased vascular resistance. Clinician’s goal is to keep MAP over 85 to maintain cord perfusion. May require pessors, atropine, pacing.
The Great Steroid Debate: 2013 American Association of Neurosurgeons state that steroid use is not recommended. Omi comment: There is no indication to give steroids in spinal cord injured patients. Many trauma centers have not been giving steroids for over 10 years. This statement by the Neurosurgery Association helps the emergency physician greatly to not give steroids.
Prognosis: C1-C3 injuries have highest risk (6.6 fold) of death. DVT is a common complication of spinal cord injury.
There was discussion of therapeutic hypothermia for cord injury. Dr. Omi felt that ongoing research would demonstrate that therapeutic hypothermia will not be helpful for complete cord injuries but for cord contusions or central cord syndrome it may be prove to be useful. Andrej comment: Recent Neurosurgical Society statement says there is no current evidence to recommend therapeutic hypothermia for cord injury.
Omi comment: It is difficult to keep a quadriplegic patient off the ventilator. They can’t cough forcefully and they have too much respiratory muscle weakness. Dr. Omi mentioned that some trauma surgeons are placing diaphragmatic pacers to avoid intubation.
Watts Study Guide Psychiatric Emergencies
Phencyclidine related seizures are resistant to phenytoin. Use benzos first. PCP is structurally similar to ketamine.
Naltrexone reduces alcohol craving and relapse without unpleasant side effects.
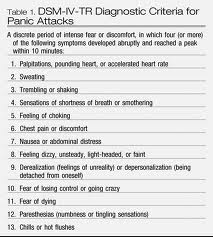
Panic attacks are characterized by discrete episodes of intense fear in absence of real danger. Patients have both somatic and cognitive symptoms. Preferred treatment for panic disorder is cognitive behavioral therapy and SSRI’s. Benzo’s are effective for short term relief. Harwood comment: Panic attack is a diagnosis of inclusion. You need 4 of 13 criteria for diagnosis. There was consensus among faculty the emergency physicians can appropriately to counsel pt’s on how to manage these attacks with cognitive/relaxation stragtegies. You may need to refer patient for management with SSRI’s. Symptoms of a panic attack can last for over an hour.
Panic Attack Criteria
Munchausen syndrome: Young to middle aged men most commonly have this diagnosis. Munchausen patients create stories about medical illnesses in order to experience medical care. Malingerers, on the other hand, act in a way to achieve secondary goals and external incentives. Harwood comment: The key is what the motivation is for the patient. If their motivation is to be the center of medical attention then it’s munchausen’s disease. If the motivation is to get drugs or get out of work then it is not munchausen’s.
Primary gain is related to a patient wanting to improve their internal feelings. Secondary gain is related to gaining advantage of external factors like getting off work, getting drugs, gaining money.
Dystonic reactions and akathesia most commonly are caused by any anti-psychotic. Treat with Benadryl and cogentin. 2nd line treatment is benzos. Harwood comment: Cogentin (benztropine) is longer acting than Benadryl so you should give the patient some. Continue Benadryl and cogentin for 2 days.
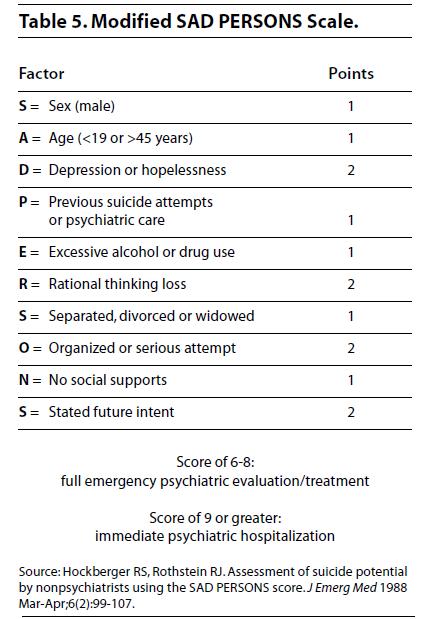
Risk of suicide: men, older, psychosis, previous suicide attempt, excessive drugs/etoh, lack of social support, serious suicide attempt. Kelly comment: Get corroborating info from family members or partner/friend. Family/friend history may be significantly different from the patient’s history.
Sad Persons Scale
Venlafaxine (Effexor) is a serotonin-norepi re-uptake inhibitor that can prolong the QT interval. Methadone can also prolong the QT interval.
Anxiety is the most common class of psychiatric disorders seen by primary care physicians.
Managing the agitated patient: Physical and chemical restraint are both needed. Document that the patient is a risk to patient and staff. There was a discussion about using chemical restraint to reduce the risk of cardiac arrest from acidosis related to agitated psychosis. Ketamine was discussed as a tool for chemical restraint. Kari Tekwani said, in her experience, Ketamin works well calm patients but some psychiatric facilities will not accept patients in transfer after being given ketamine. Also there was a discussion about the differences between geodon and haldol for chemical restraint. Consensus was that their effectiveness/risk was largely equivalent.
Treatment of Neuroleptic Malignant Syndrome: Stop anti-psychotic, IV fluids, cooling, benzos, consider dantrolene or bromocriptine. Classically patients have lead pipe rigidity, hyperthermia, autonomic instability, and mental status changes. Differential includes serotonin syndrome.
Ryan Med Student Review
