Hey everybody, Another great week of very clinically relevant EM discussions. Enjoy!
Collander/E Kulstad Oral Boards
Case1. 14 week old infant breathing funny per mom. RR=58 HR=240 PO=95%. EKG shows SVT. Critical actions were to get an EKG, diagnose SVT, and treat the rhythm. Erik comment: Current recommendation in SVT for infants is to get a 15 lead ekg that includes 2 right sided leads and 1 posterior lead. 50% of kids with SVT don’t have structural heart disease. 93% do not require ablation. Infants can tolerate SVT for up to 24 hours prior to developing CHF. You can initially try vagal maneuvers (take a rectal temp, place ice bag on face, DO NOT do carotid massage in kids they can develop asystole). Adenosine is drug of choice. Calcium channel blockers are contraindicated for SVT in kids. Cardioversion is your back up plan.
Case2. 32yo male with flank pain and fever. Patient had urosepsis and ureteral stone. Critical actions: Diagnose kidney stone and signs of urosepsis. Initiate IR decompression of infected kidney and/or urologic removal of ureteral stone. Start IV antibiotics. Erik comment: IR drainage of a kidney usually takes less time and maybe should be your first move in the sicker, older patient. Either IR drainage or Urologic procedure to remove stone will decompress the kidney and solve the problem. Pursue whichever option you can get faster at your institution.
Case3. 44yo female with chest and leg pain. Diagnosis was thoraco-abdominal aortic dissection with extension into the superior mesenteric artery. The dissection occludes the left common iliac artery. Initiate medical management with esmolol first followed by nitroprusside or nicardipine. Emergently consult for surgical management of aortic dissection. Pain control.
Elise comment: For the boards, get IV started right away in patients with abnormal vitals. Watch your time when doing the physical exam. You have to balance completeness with being efficient. The case will end when the time is up so be conscious of your time. Adenosine dosing is 0.1mg/kg followed 0.2mg/kg if first dose fails. Chest pain plus anything else(vascular symptoms, stroke symptoms, abdominal pain, any other symptom)=aortic dissection. Be aware that betablockade in the face of cocaine use may result in unopposed alpha effect. Esmolol is a good choice to avoid this because you can turn it off rapidly due to it’s short half life.
Harwood comment: You don’t do EP studies in kids less than 5 years due to risk of death during the procedure. When IR gets involved in an infected/obstructed kidney, they percutaneously drain the pus from the kidney. After that is done, urology can transurethrally go in to remove the stone.
Paquette Study Guide Special Patients
Black tar heroin is associated with fungal endophthalmitis (fever, visual changes).
IV heroin and IV cocaine are both associated non-cardiogenic pulmonary edema. It will usually resolve in around 24 hours with support with bipap or mechanical ventilation.
Cotton fever is due to the pyrogenic material in cotton that enters the IV drug user’s bloodstream if they filter their heroin with cotton balls.
Cocaine is a more frequent cause of endocarditis than heroin due to: shorter half life, more frequent injections, and the fact that it is not heated prior to use.
Trench foot is due to prolonged skin exposure to water (wet socks and shoes) which causes stratum corneum breakdown.
Subdural hematoma is more common than epidural hematoma in the elderly. This is due to smaller brain and fragile bridging veins. Subdural hematoma is associated with greater underlying brain injury than epidural hematoma.
30% of trauma deaths occur in patients greater than age 65 despite the fact they account for less than 20% of injuries.
Treatment of maggots: there was a discussion about this but 3 approaches were discussed. 1. Ethyl chloride either directly on the wound or in a bag in which the limb is inserted. 2. Immersing the limb in betadine. 3. Yankauer suction of maggots from the wound.
The most commonly missed fracture in the ED is the second fracture.
Autonomic dysreflexia: You get unopposed sympathetic response to some noxious stimuli in a paralyzed patient. Uti is most common cause. Fecal impaction or bowel obstruction are the second most common cause. Treat the cause and manage the BP.
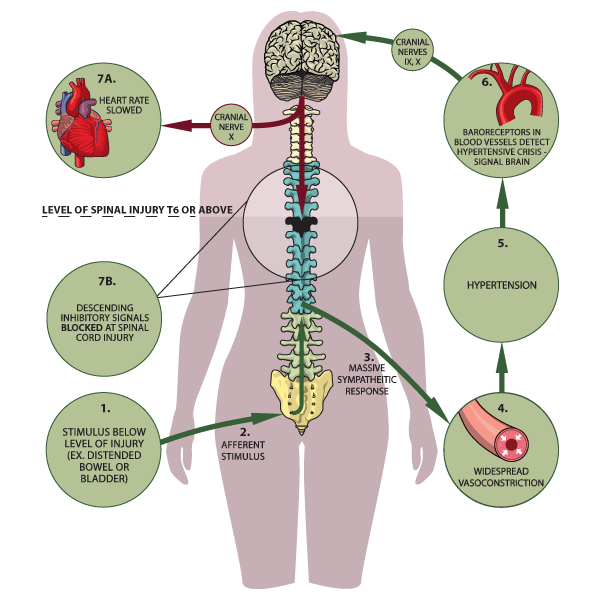
Autonomic Dysreflexia
Wernicke’s syndrome: Thiamine deficiency causes occulomotor dysfunction, cognitive dysfunction, and ataxia.
EKG’s in the morbidly obese consistently show flattening or T wave inversion in the infero-lateral leads.
Down’s patients have atlantoaxial instability. Girzadas comment: this makes Down’s patients at greater risk for spinal cord injury in trauma.
Heterotopic ossification can be due to trauma, spinal cord injury, severe neurologic disease, burns and rarely to genetics. The cause is unknown but alkaline phosphatse is thought to play a role. Patients will have warmth, tenderness and swelling initially at the site of heterotopic ossification. The hip is probably the most common site. The affected site is always below the level of the cord lesion.

Heterotopic ossification
Garret-Hauser Ethics
Case 1. Trauma pt was driver in MVC with girlfriend who was passenger and also injured. Male Pt (driver) is HIV positive. Both he and girlfriend are admitted with injuries. There was extensive blood at scene. Patient has asked that his girlfriend not be told about his HIV status. Treating MD obviously very troubled by this situation. Strategy: Discuss with HIV positive patient about his obligation to his girlfriend. If he refuses to give this information to his girlfriend, then counsel the girlfriend that she was exposed to unkown blood and she should receive prophylaxis. Elise comment: The female patient likely has been having sex with the male patient and she needs an HIV test. Harwood comment: Tell the patient we have some information that we can’t pass on to you that makes us strongly advise you to receive HIV prophylaxis. You can also say you were exposed to HIV positive blood. Shayla comment: The hospital has to report to the health department that the male patient is HIV positive. The health department will eventually notify the patient’s girlfriend.
Case2. 15yo female is pregnant and parent doesn’t know. Kelly comment: First figure out if there is any issue of safety for the girl if she reveals to family she is pregnant. Shayla comment: Get the closest responsible female from the family to help in this situation. Encourage the girl to disclose the information to the parent while still in the ED. If the girl refuses, you can tell the parents there are test results that your daughter refuses to allow me to discuss with you. If you want to discuss this issue with your daughter now, I will be here if you want to discuss. Also, you can advise parents that they can request the medical records.
Case3. Mom demands drug testing on her son. If the child agrees to give urine, the results of the drug screen are not protected information and can be given to the parents. The American Academy of Pediatrics recommends against drug testing outside of the primary care physician’s office. Attending consensus: Most would not force a catheter or a pelvic exam or draw blood on an actively refusing patient. There is no medical emergency in a well appearing patient. If the child agrees to testing then most would do the test for the parents. If parents request a genital exam to evaluate if a girl had sexual activity, our female faculty all would refuse to inflict this exam on a girl.
Case4. 59yo male found unresponsive after intentional overdose. Pt has terminal lung cancer. He has DNR/DNI. Discussion of whether or not pt should be resuscitated. Consensus was that you have to intubate patient or try narcan and flumazenil. But not actively resuscitating the patient would be akin to aiding a suicide. Although some states have legal physician assisted suicide, the AMA still opposes physician assisted suicide. Elise comment: not resuscitating this patient places you at very high legal risk and high ethical risk. You gotta resuscitate the patient. Christine comment: We are not required to provide medically futile care, so if a patient shots himself in the head you may not need to try to resuscitate that patient if the prognosis is futile. Girzadas comment: For the patient who overdosed, I would way rather be defending myself on the side of resuscitating him versus letting him die.
Putman M&M
Elderly male with SOB. Code 44 on arrival. O2 sat is 76% and HR=120, normotensive and afebrile. Lungs are clear. Pt was incontinent of heme positive stool. Bipap started. IV PRBC’s given. Niece gives history of abdominal pain and diarrhea and coffee ground emesis. Pt has myelodysplastic syndrome and is on warfarin among other meds.
Hgb=7.2, ABG=7.44/19/148/12, Lactate is 7, Bun/cr=117/3.5, INR result was delayed. CT was ordered.
Work up proceeds over next 1-2 hours. Patient at one point arrests. ROSC obtained with intubation, epi and more IV prbc’s. Elise comment: LMA may have been sufficient during code. Harwood countered that intubation in this patient with hx of coffee ground emesis is very reasonable during code.
INR is still pending. A call to lab revealed that the INR result was not reported because it was too high to be calculated. When this was learned FEIBA and vitamin K were administered. Pt received octreotide and pressors as well. Patient coded multiple times and family withdrew care and patient died.
Lessons:
Coags are a critical piece of info in the GI bleeding patient. If there are significant delays, we need to investigate what is delaying the result. Multiple attendees asked why questionable or extreme results can’t be reported to the physician. We need to know about these time critical results. Mila comment: there is a system wide initiative to develop a plan for this problem.
Discussion of placement of NG tube in this patient: Consensus that it would have not have helped much. Harwood comment was that NG can help diagnose UGI bleeding but you already knew the patient had an UGI bleed. It can also help you quantify UGI bleeding but you were already giving blood and knew the patient had a significant bleed. Girzadas comment: NG aspirate has a high false negative and false positive rate so it could potentially have lead you to think the bleeding was less severe than it actually was.
There was a discussion of the use of bipap in this case. Bipap can insuflate air in the stomach and exacerbate vomiting. Group consensus was that bipap was reasonable and helped the patient. Christine comment: I would have tried bipap in this patient also, but maybe intubation is the better plan of action to avoid gastric distension. Erik comment: Historically in the past, we used to tube more GI bleeders. Elise comment: Trust your gut if your feel that a patient is critically ill and secure the airway.
Kelly comment: You are the managing physician of the patient. Be clear about what you want a consultant to do. Lead off your conversation with what you need from your consultant and follow that with further detail of the case.
Harwood comment: I am ok with giving FEIBA in this case without the INR result. The patient was known to be on warfarin with a recent therapeutic INR as an outpt, anemia, and obvious current GI bleed. You can tell GI or IR that you are giving FEIBA and the INR will likely be reversed in about 30 minutes so they can start coming in to do endoscopy. Sam Lam comment: U/S may have been helpful to rule out other intra-abdominal emergencies.
It was discussed that some consultants and other ED’s use gastric lavage as a decision making tool for upper GI bleed. NG tube placement is safe in the setting of esophageal varicies.
PPI’s have been shown in Cochrane review to not improve mortality, re-bleeding, or surgery in undifferentiated UGI bleed. It does show that signs of serious bleeding are less on endoscopy following PPI use. SMARTEM podcast did not feel PPI’s were beneficial in UGI bleed. There is a Cochrane review of PPI’s for specifically peptic ulcer disease related bleeds that showed no mortality benefit but there was less rebleeding and less surgery required.
Sangstaken-Blakemore tube. Harwood comment: The only situation that has theoretical benefit with this device is esophageal variceal bleeding. There is a problem that you need to keep tension on the tube to keep stomach balloon compressing the upper stomach. Traditionally people have used foot ball helmets in order to tether the tube to the facemask. Some attending have tethered the tube to a bed railing.
Activate the massive transfusion protocol in the critically ill GI bleeding patient.
Blachford Scale can be a useful tool to identify low risk and high risk UGI bleeders.

A journal club on this scoring system within the last 18 months found that with a score of 2 or less and age <70, patients could be considered for possible D/C. A score higher than 3 likely would need an intervention.
Febbo Safety Lecture Diagnosing DKA
24yo female , 13 weeks preg presents with vomiting. Pt has an insulin pump for DM. Glucose was 133. Anion gap=21. ABG has a PH of 7.54, PCO2 is 19 and HCO3 is 16. Pt has some respiratory alkalosis and metabolic acidosis. Ketones in urine was >80. UA showed signs of UTI.
Pt was treated with IV fluids & IV antibiotics and labs improved with nl anion gap and bicarb up to 19. Pt was admitted and Insulin pump was turned off per hospital standard practice. Overnight on the floor, pt did not receive any insulin. In am next day, anion gap had increased and ph dropped. DKA was diagnosed and pt was transferred to the ICU. Harwood comment: There is no mystery here. A pregnant, diabetic patient with a UTI needs insulin. With no insulin, she will develop DKA. Theresa Navarette comment: In a patient with DKA, turn their pump off because it could be malfunctioning and treat the patient with IV insulin. In a patient without DKA who has an insulin pump it is reasonable to keep using the pump because it is probably working based on controlled blood sugar. There was consensus that a shot of Lantus insulin prior to the patient going up to the floor may have prevented the patient going into DKA. Maggie comment: Endocrine is more than happy to consult on patients with insulin pumps.
