Conference Notes 10-1-2013
Be safe out there! Be careful with sharps.
Maletich/Anderson Oral Boards
Case 1. Adult Epiglottitis; pt presented with severe sore throat and forward leaning posturing. Lateral neck xray showed enlarged epiglottis. Pt maintained a patent airway and did not require intubation/cricothyrotomy Critical actions: IV antibiotics, ENT consultation, prepare for any airway compromise by having both advanced intubation options (direct and video laryngoscopy) and a surgical airway option ready. Racemic epinephrine is another option to reduce epiglottis edema.
Case 2. Pt presented with hypoglycemic seizure and altered mental status. Diagnosis was panhypopituitarism due to previous surgery of pituitary gland. Patient was on vacation and was not taking her usual medications. Critical actions: IV fluids, treat hypoglycemia, IV hydrocortisone , management of hyperkalemia.
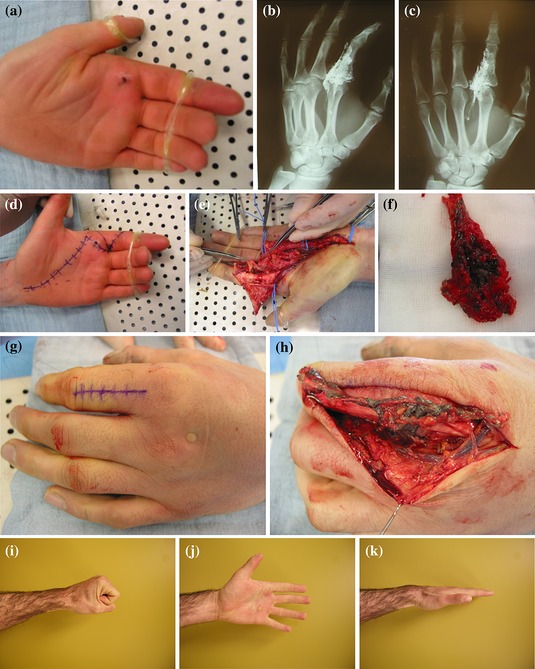
Case 3. 38yo male struck in mouth with baseball bat while coaching kids little league. Tooth was completely avulsed. Critical actions: Place tooth in Hank’s solution (Save-a-Tooth) until reimplantation, attempt reimplantation of tooth, consult Oral-Maxillofacial Surgery. Get tooth in the socket as soon as possible. Do not scrub tooth. Only rinse tooth gently with saline. Alternative mediums to transport an avulsed tooth include chilled milk, and saliva.
Elise and Harwood comments: You have other options to lower fever besides oral or rectal acetaminophen. You can use IM/IV ketorolac or in kids, you can use IV acetaminophen.
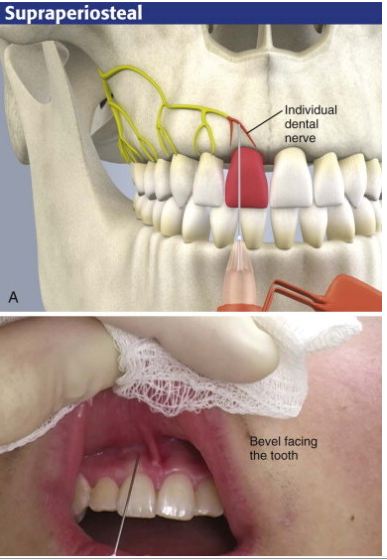
Elise comment: appropriate local anesthesia to replace an avulsed tooth requires injection of anesthetic around maxillary ridge (supraperiostial injection). Infraorbital nerve block does not provide adequate anesthesia of maxilla or tooth socket.
Roberts and Hedges’ Text:
The most common technique for intraoral local anesthesia of individual teeth is supraperiosteal infiltration (Fig. 30-5). This technique can provide complete relief of a toothache. Select the area to be anesthetized and dry it with gauze. Apply a topical anesthetic, such as 20% benzocaine or 5% lidocaine ointment, as described. Ask the patient to close the jaw slightly and relax the facial musculature. Grasp the mucous membrane of the area with a piece of gauze. Pull the gauze outward and downward in the maxilla and outward and upward in the mandible to extend the mucosa fully and to delineate the mucobuccal fold. Puncture the mucobuccal fold with the bevel of the needle facing the tooth. Aspirate the area and deposit approximately 1 to 2 mL of local anesthetic (2% lidocaine should be used here) at the apex (area of the root tip) of the involved tooth (see Fig. 30-5). It is helpful to place a finger against the outer aspect of the lip overlying the injection site. Apply firm and steady pressure against the lip and slowly inject the local anesthetic into the supraperiosteal site. This helps prevent ballooning of the lip.
The purpose of the injection is to deposit the anesthetic near the bone that supports the tooth. The anesthetic must penetrate the cortex of bone to reach the nerve of the individual tooth, so the injection may fail if the solution is deposited too far from the periosteum, if the needle is passed too far above the roots of the teeth, or if the bone in the area is unusually thick or dense. If anesthesia is unsuccessful, inject the palatal side. It may take 5 to 10 minutes to achieve full anesthesia with this technique, however, and the procedure may not be as effective for the posterior molars. Infiltration of the area around the maxillary canine and the first premolars will anesthetize the MSA and ASA nerves; lacerations of the upper lip can be treated by bilateral injection in the canine fossa areas.
Balogun Trauma Lecture
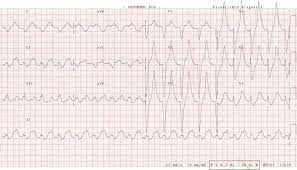
Blunt poly-traumatized patient due to motorcycle accident transferred to ACMC. Pt had LMA placed in outside hospital and had a cardiac arrest at outside hospital prior to transfer to ACMC. Pt had massive free fluid in peritoneal cavity on FAST exam. Pt had cardiac arrest in ED. Pt was intubated and bilateral chest tubes were placed. PRBC’s were transfused. Pt had severe facial trauma and had nose packed multiple times for severe epistaxis. OR was not immediately available due to 2 other trauma cases going at the time. Massive transfusion protocol was initiated. Patient arrested again and was resuscitated with ACLS. Pt develops a massive neck hematoma. Patient continued to bleed profusely from head/facial injuries. Pt had pelvic binder placed for widely diastatic pelvic fracture.
Elise comment: At some point you have to decide if utilizing massive resources to further attempt resuscitation is futile.
Sola’s response: That is exactly correct. The trauma attending evaluated the patient and when pt again arrested the decision was made that further resuscitative efforts were futile.
Altered mental status or agitation can be a sign of shock.
(Up to Date) The Advanced Trauma Life Support (ATLS) manual describes four classes of hemorrhage to emphasize the early signs of the shock state [3]. Clinicians should note that significant drops in blood pressure are generally not manifested until class III hemorrhage develops, and up to 30 percent of a patient's blood volume can be lost before this occurs:

Girzadas comment: Class 1=10% (500ml) blood loss (no change in vitals), Class2=20% (1000ml)blood loss (tachycardia), Class 3=30% (1500mL) blood loss (hypotension/mental status change), Class 4= 40% (2000ml) blood loss (hypotension/altered mental status/minimal urine output).
No evidence favoring either NS or LR for resuscitation.
Massive Transfusion Protocol: 1:1:1 transfusion ratio of of PRBC’s: FFP: Platelets. Here at ACMC the massive transfusion protocol can be activated by a Trauma attending or an ED attending. Elise comment: as a resident you have to really push to get the blood products into the patient. You have to place order in care connection and call blood bank at (41-5581) Nurse must send a “Blood Release Request” in order for blood to be released. Christine comment: Have a tech run this form down to blood bank and bring the blood products back. Massive transfusion protocol gives the patient 10 units of prbcs, 6 units of FFP, 1 unit of apheresis platelets, 2 units of cryoprecipitate. The first 4 units of prbc’s of the massive transfusion protocol are O-neg prbc’s that are sent to ED immediately. Use the level 1 rapid warmer/infuser to give fluids and blood rapidly.
No human studies support the use of vasopressors in the resuscitation of trauma patients. Elise comment: If patients with hemorrhagic shock are on pressors, stop the pressors. If they aren’t on pressors, don’t start them. Give blood.
There was a discussion of using IO lines for prbc transfusion. Consensus was that IO lines are an ok way to give prbc’s but not as effective as large bore iv lines. Roberts and Hedges reference a rate of 21 ml per minute for prbc transfusions via IO versus 35 ml per minute transfusion rate via large bore IV.
Tranexamic acid: CRASH-2 showed lower mortality overall in trauma patients and lower death from hemorrhage. Best if given in the first 3 hours. 1g IVPB over 10 min followed by 1g IVPB over 8 hours. You can’t give this in the same line as blood products. TXA is not indicated for isolated head bleeds. Elise: Give this in the first three hours in patients who are hemorrhaging or who you expect to need blood transfusion. Harwood comment: TXA can also be used for gynecologic bleeding. Kelly comment: I had a patient who requested TXA for gyne bleeding. She had received TXA for severe vaginal bleeding previously Elise comment: OB attendings here feel there are other options preferable to TXA for vaginal bleeding.
Opportunities for improvement indentified by Sola:
Get control of scalp lacs and epistaxis. Use a staple gun to close scalp wounds. Harwood comment: consider using hemecon or some other material promote coagulation to control severe nasal bleeding. Christine comment: You may consider posterior balloon to stop epistaxis. Harwood comment: be careful with placing objects in the nose when you suspect there are mid face fractures so that you aren’t placing a catheter into the brain.
Be diligent with placing the pelvic binder and check it regularly to make sure it is in proper position. Activate the massive transfusion protocol early (as soon as patient arrives in ED). Control hypothermia with arctic sun device or bear hugger. Get help from ED resources to help manage these difficult cases. Elise comment: Please ask the ED attending for guidance and help with these resuscitation if the Trauma attending is in the OR. Harwood comment: Nice job intubatiing this patient with massive facial injuries. Some brain injuries are associated with coagulopathies and that may have been a factor in his hemorrhage. IR may have been an option to embolize his pelvic vessels or his spleen. Trushar comment: If you are at a non-level 1 ED, get a patient such as this out of the ED rapidly. Maybe intubate them and get blood stated and get them out. Erik comment: Don’t do any work up at the transferring hospital, just get them out to the receiving hospital ASAP.
Mistry Study Guide Administration
Occurrence-based malpractice insurance policies cover you for events during the policy period regardless of when the claim is made. Claims-made policies cover you only when the policy is in effect. So with claims-made policies you need to purchase a tail to cover you for any claims made after the policy ends. A Claims-made policy plus tail coverage effectively becomes an occurrence policy.
Insurance distributes risk over a large group.
If you are sued more often than the average physician you are flagged by insurance companies.
A simple made up word to remember charting requirements: “Fourtwoteneight” (pronounced 4-2-10-8 say it fast) Four HPI elements, two past med/ family/surg/ social history components, Ten ROS systems, eight physical exam components are what is needed for a level 5 chart.
Boarding increases the rate of patients who leave without being seen. Boarding does not affect the waiting times of critically ill patients but it does affect the waiting time of less ill patients.
Criteria for deiversion: No inpatient telemetry beds open. ED is overwhelmed by patients or other problems such as electrical failure or water main breakage. If all the hospitals in a region go on diversion, then all the hospitals in that region have to go off diversion.
Consent for minors: Attempt to contact the parents but if the patient’s health is at risk do the right thing and treat the patient while attempting to contact the parents. In fact, most routine, indicated care can be started while you are attempting to contact the parent. You definitely can perform the EMTALA screening exam prior to getting parental consent. Emancipated minors are those that are married, pregnant, minor who is a parent, minor who is in the military. Emancipated minors do not need parental consent to begin treatment.
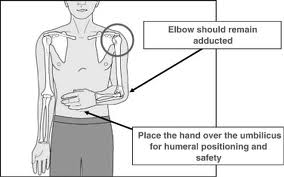
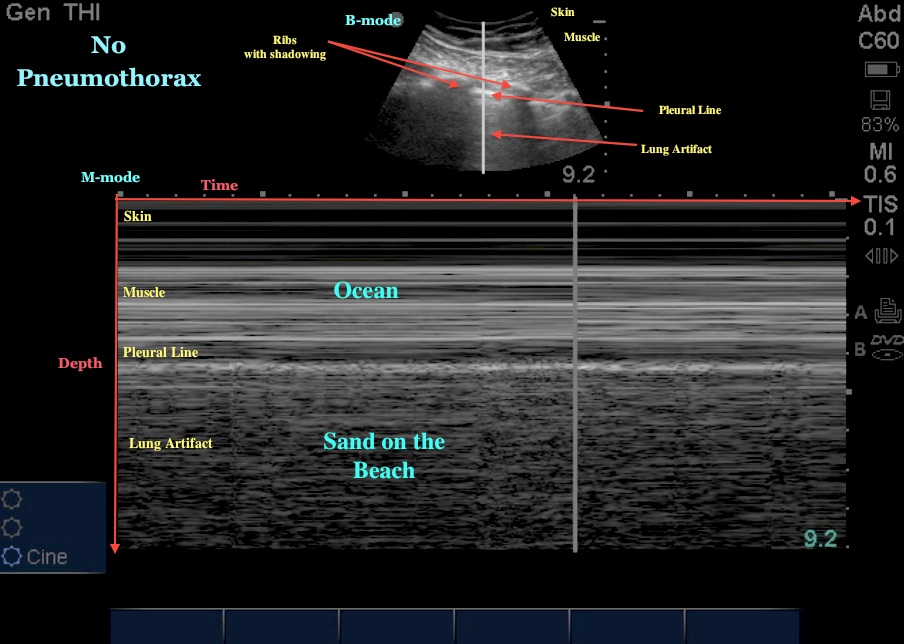
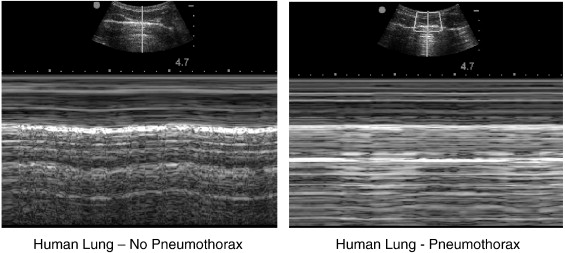
Chiefs/Faculty Joint Aspiration and Reduction Lab
5 Stations: 1. Shoulder, 2. elbow/knee, 3. wrist, 4. Hip, 5. Ankle
Have a good week everybody!